
This new digital journal has been developed to help you to excel in your job at a time when the demands made of you have never been greater.

Helen Lake describes and reflects on the first year of a nurse-led, public-facing urinary tract infection (UTI) information service and considers its relevance for nursing practice.
Helen Lake is Urology Specialist Nurse and UTI Information Nurse, The Urology Foundation
For many patients living with digestive conditions, the anxiety of being caught short in public can be as debilitating as the physical symptoms themselves. Guts UK, the national charity for the digestive system, launched their “Can’t Wait” card to address this barrier to independence and improve patients’ quality of life.

Children with Down syndrome can be affected by a number of different bowel conditions. June Rogers explains what these conditions are and how they can be managed.

Dr Nicola Adanna Okeahialam, Professor Fiona Reid
Women presenting with stress urinary incontinence or pelvic organ prolapse face an increasingly complex landscape of treatment options. Owing to a lack of clear superiority between treatment options for pelvic organ prolapse and stress urinary incontinence, the decision about which surgical procedure will be performed is a ‘preference sensitive’ decision, requiring careful consideration of each patient’s values and goals. However, the process of making a decision about treatment can be challenging because of a number of factors including patient understanding, clinician preferences and institutional barriers. In line with principles outlined in Montgomery v Lanarkshire Health Board [2015] and following the recommendations of the Cumberlege report, a collaborative approach to shared decision making is essential, to identify both what matters most to patients and also the material risks. This can be achieved by using patient decision aids to supplement consultations and support patients to reach an informed and preference-sensitive decision regarding surgery.

This series of short videos from our editors collates their top tips for writing and publishing articles into one easy-to-access guide. Have a look and they might inspire you to get writing.
With the prevalence of dementia increasing, and better understanding of its links with bowel and bladder problems, a new leaflet from Bladder & Bowel UK gives an overview of ways to maintain bladder and bowel health in people living with dementia, and discusses how to prevent or reduce incontinence in this group.
Updated guidance on catheter care from the Royal College of Nursing is a resource for any healthcare professional who is required to undertake urinary catheterisation as part of their role. Intended for use in both teaching and practice, it combines evidence with clinical experience and expert opinion.
This two-part series explores why a good balance of microbiota is important and what factors encourage a healthy microbiota and what factors cause an imbalanced one. This first article outlines why the gut microbiome is so important for health and wellbeing and what an unbalanced microbiota (otherwise known as dysbiosis) can lead to.
Key words: Gut microbiome; Physical and mental wellbeing; Healthy microbiota; Dysbiosis; Gut–brain axis

In a companion piece to their previous article, Abdul Seckam, Stephen Mitchell and Heidi V Tempest discuss the benefits and challenges of using teleurology and outline a case study where their digital urology service was used to address a backlog of patients waiting for a urology assessment.
RCN report outlines impact of nurses remaining on lower bands on career progression, staff retention and patient care.

While it has long been known that black men have a higher lifetime risk of dying from prostate cancer, a new analysis by Prostate Cancer UK has shown that ethnic disparities persist at every socioeconomic level, with black Caribbean men consistently facing the greatest burden. The analysis concludes that increased mortality from prostate cancer among black men cannot be explained solely by socioeconomic factors.

New guidelines from the Department for Health and Social Care have been published. Their aim is to improve the quality of alcohol treatment so that people with patterns of harmful drinking and alcohol dependence get better help and support and achieve better outcomes.
EFUNCore, a core educational framework for urology nursing, was launched at the British Association of Urological Nurses (BAUN) conference in Edinburgh last month. Devised, constructed and agreed as a partnership between four international urology nursing associations – BAUN, the European Association of Urology Nurses, the New Zealand Urological Nurses Society and the Australia and New Zealand Urological Nurses Society – the document is a step forward in the education of urology nurses.

Up to 30% of children are affected by constipation at any one time. In this article, June Rogers highlights the importance of early intervention and looks at the evidence for the different management and treatment options. This follows on from her previous article looking at the factors that contribute to childhood constipation.
An updated consensus statement from the British Menopause Society is now available on the topic of genitourinary syndrome of menopause, updating the previous guidance on urogenital atrophy.
New guidance from NICE (the National Institute for Health and Care Excellence) gives another treatment option for people with hormone-sensitive metastatic prostate cancer for whom docetaxel is not suitable. The guidance discusses the use of darolutamide with androgen deprivation therapy for treating hormone-sensitive metastatic prostate cancer.

While men with symptomatic benign prostatic hyperplasia (BPH) are normally treated with medication, approximately 10% of men with BPH eventually require surgical intervention. In this article, the second in a two-part series, Linda Nazarko discusses the minimally invasive and invasive surgical options for treating BPH.

Constipation occurs in around a third of children, and more of those with Down syndrome and other learning disabilities. June Rogers explains how constipation can develop during different points of a child’s life and how this can be treated. An accompanying article looks at treatment options.

New guidance funded by the British Dietetic Association, and produced by a team of UK-based clinicians, gives the first comprehensive evidence-based dietary guidelines for the management of chronic constipation in adults.

Jennie Burch, head of gastrointestinal education, St Mark’s Hospital
Learning to live with a stoma and adapt the stoma into lifestyles can be difficult, and community nurses are well placed to provide information about travel to people living with a stoma. Patients often want advice and reassurance that they can travel, and nurses can direct them to reliable sources of information. Community nurses can encourage travelling as a safe and enjoyable way to live after stoma forming surgery.
Key words: Stoma, Travel, Planning, Challenges, Signposting
A number of areas of the National Institute for Health and Care Excellence (NICE) Clinical Knowledge Summary on Prostate Cancer have been updated in light of new research. Make sure you know what the latest recommendations mean for your patients.
By: Ross Othen-Reeves
With Stoma Awareness Day happening on 4 October, Ross Othen-Reeves highlights the work that Colostomy UK is doing and introduces their new Stoma MythBusters campaign.
By Laura Noble, Bladder Cancer Clinical Nurse Specialist, Department of Urology, Freeman Hospital, Newcastle
Bladder cancer affects over 20 000 people each year in the UK. This article outlines changes made to the bladder cancer pathway to ensure patients are diagnosed and receive treatment as soon as possible, and the impact this has had on speeding up the process and freeing up nursing time.

Indwelling urinary catheters are commonly inserted in hospital and an estimated 90 000 people living in the community have indwelling urinary catheters. One complication of urethral catheterisation is meatal pressure injury, also known as iatrogenic hypospadias. Both men and women can suffer a meatal pressure injury, but this article examines why these develop in men and how to prevent, recognise and manage these injuries.
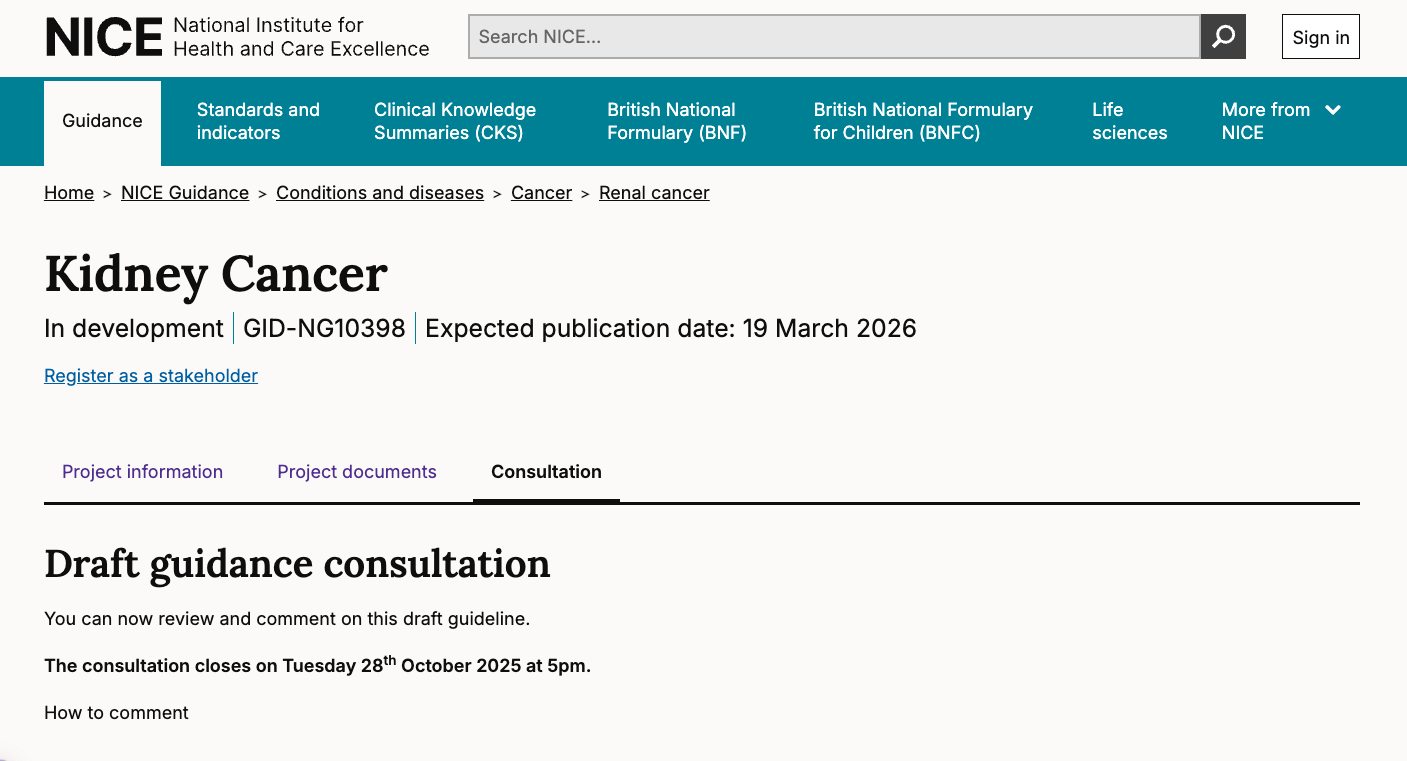
You have until 28 October to comment on the draft NICE (National Institute for Health and Care Excellence) guidance for the diagnosis and management of renal cell carcinoma in adults. The guideline aims to improve care by helping healthcare professionals offer people the right treatments and support, taking into account the person’s individual preferences.
.jpg)
Benign prostatic hyperplasia (BPH) is thought to affect over 3.2 million older men, yet only 400 000 are treated for this condition (UK Parliament, 2009). Some men may experience mild symptoms that they are able to manage while others may be too embarrassed to seek treatment or be unaware that there are treatment options (Emberton et al, 2008).
This article, one of a two-part series, outlines why BPH develops, how men can reduce their risk of developing BPH and discusses the non-invasive treatment options available. The second article, which discusses the minimally invasive and invasive surgical options for treating BPH, can be found here.
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved gepotidacin (Blujepa), a new kind of oral antibiotic pill to treat uncomplicated urinary tract infections (UTIs) in females aged 12 years and older, weighing at least 40 kg.
Author: Debbie Gordon, Head of Commercial Services & Education, ERIC
It’s Urology Awareness Month in September and the theme this year is ‘time to act’. ERIC, The Children’s Bowel & Bladder Charity, has been doing just that, undertaking an extensive content project to make continence advice more accessible to families who really need it – but we need more support.

Author: June Rogers MBE, Independent Children's Bladder and Bowel Practitioner
The human gastrointestinal tract contains the body’s largest community of microbes, comprising trillions of microorganisms collectively referred to as the gut microbiota. Disruption or imbalance in the gut microbiota may result in dysbiosis or leaky gut syndrome. Dysbiosis has been linked to a range of diseases in both children and adults, including autism spectrum disorder, attention deficit hyperactivity disorder, asthma, and various allergies.
One-piece closed bags for colostomies: late-stage assessment, the latest health technology evaluation from NICE (National Institute for Health and Care Excellence), was published earlier this month.
Author: Catherine Best, Visiting lecturer in nursing, Birmingham City University, Birmingham
‘Wicked’ problems, a term for complex, challenging issues, are inherent in healthcare, and it can be argued that they exist in all areas of life. Yet, it is possible to provide solutions to these problems by understanding the complex nature of inter-process communication, inter-professional collaboration and shared commitment, the successful application of which has the potential to bring about positive change.

An estimated 90 000 people living in the community have long-term indwelling urinary catheters (Gage et al, 2017). Most urinary catheters are initially inserted in hospital (Shackley et al, 2017). In some cases, there are plans to carry out a trial without catheter (TWOC) but in other cases the indication for urinary catheterisation is unclear and/or there are no plans to remove the catheter. Around 50–70% of people with long-term catheters experience problems such as bladder pain, catheter leakage, blockage and urinary tract infection (Youssef et al, 2023). In the past TWOC was routinely carried out in dedicated hospital clinics (Tay et al, 2016), but in recent years increasing numbers of TWOCs have been carried out in the community (Logan and Coghlan, 2022). Suprapubic catheters are often inserted when it is difficult to catheterise urethrally and there can be the sense that suprapubic catheters are permanent (British Association of Urological Surgeons (2025). This article explores suprapubic TWOC in community settings.

By: Maya Pote, Therapy Lead, Ealing and Northwick Park Hospitals, London North West University Healthcare NHS Trust; Victoria Jones, Principal Physiotherapist, MSK & Pelvic Health, London North West University Healthcare NHS Trust
UCCT is exploring the roles of the different professions of the multidisciplinary team. Maya Pote talks to Victoria Jones about the role of physiotherapy, and what she wishes her patients and her colleagues knew about physiotherapy and pelvic health.

Urinary symptoms are unusual in healthy young adults, especially in men. This is changing as a result of increased recreational use of ketamine and its effects on the urinary system. This article highlights the clinical features of ketamine-induced uropathy and outlines treatments.
Intermittent urethral catheters for chronic incomplete bladder emptying in adults: late-stage assessment, the latest health technology evaluation from NICE (National Institute for Health and Care Excellence), is published today, 9 July 2025.

This World Continence Week (16-22 June) ERIC, The Children’s Bowel & Bladder Charity have launched a campaign with TV star Mollie Pearce and 8-year-old Katie Thirling, who both have stomas, to raise awareness and break the stigma around bowel and bladder issues.
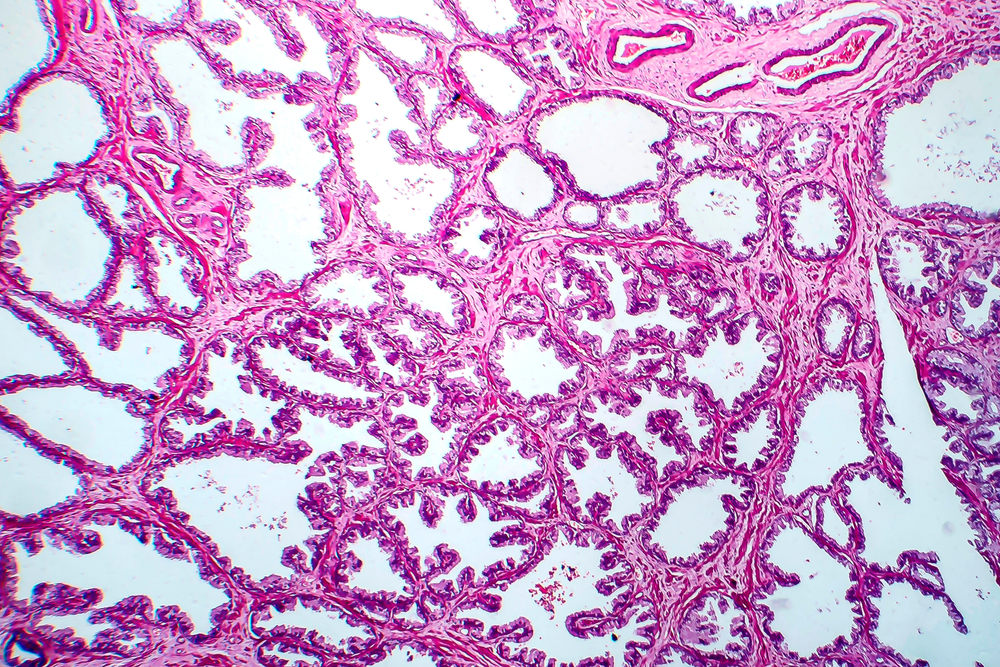
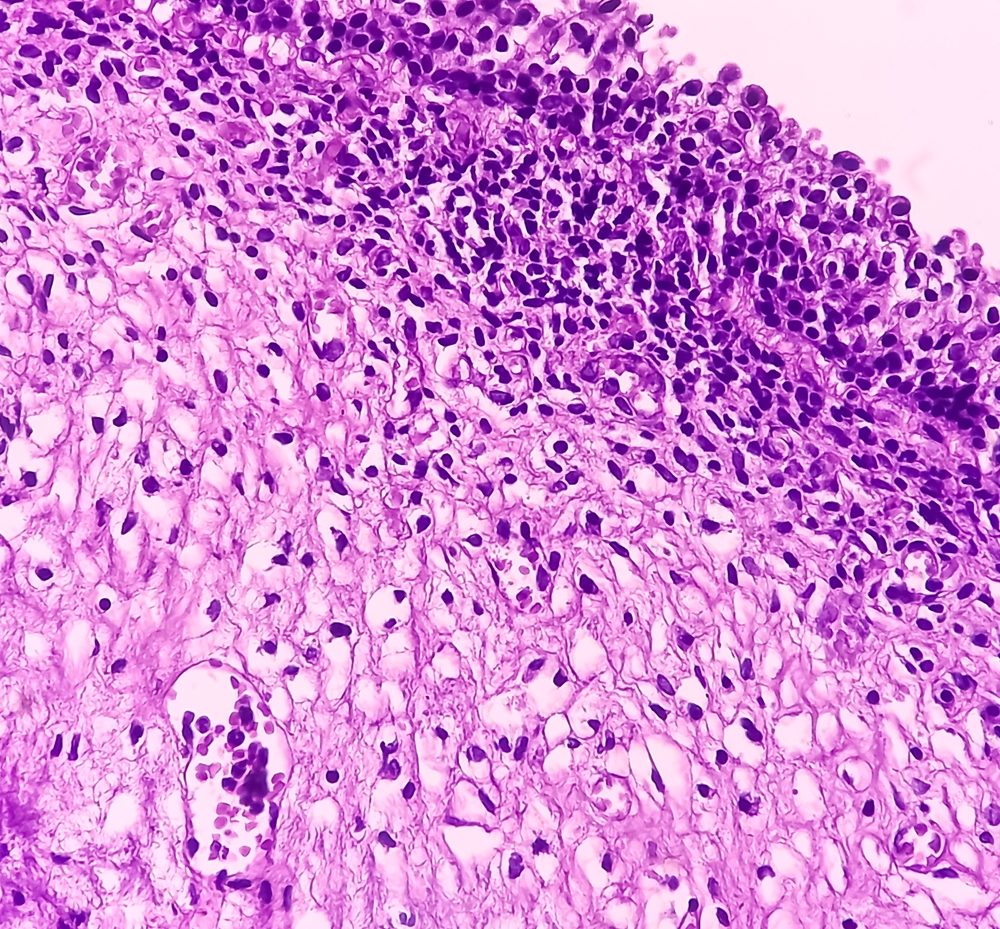
Around 10,500 people are diagnosed with bladder cancer in the UK every year. It's the 11th most common cancer in the UK, and the 7th most common cancer in men (Cancer Research UK, 2025a). Bladder cancer is most common in older people. Almost 60% of new cases are in people aged 75 years and over, and it is rare in people under 40 years of age. More men than women get bladder cancer. This may be because more men than women have smoked or been exposed to chemicals at work in recent decades (Cancer Research UK, 2025a).

With a quarter of children now starting school not toilet trained, ERIC, The Children’s Bowel and Bladder Charity is launching an intervention to help reverse the trend, and is inviting families and healthcare professionals to hop aboard the Toilet Train.
Over the last century, the average age that children are being potty trained in the UK has risen from 12–18 months, to an average of around three or even four years today (Blum et al, 2004).

Over the past few decades, advances in technology have revolutionised the field of urology. From diagnostic tools to surgical techniques, these innovations have greatly improved the way urological conditions are diagnosed and treated. The integration of technology into urology services has revolutionised diagnosis, treatment and patient care. From advanced imaging techniques to minimally invasive surgical procedures, technology plays a crucial role in improving outcomes and enhancing patient experience in urological care. This article discusses a number of these innovations and looks at how they are influencing urology practice.

Intermittent catheterisation is considered the gold standard for urine drainage (Holroyd, 2018). It can be used as treatment for voiding problems due to disturbances or injuries to the nervous system, non-neurogenic bladder dysfunction, or intravesical obstruction with incomplete bladder emptying (Royal College of Nursing [RCN], 2018). Irrespective of the underlying cause, patients with voiding problems frequently find themselves having to make use of a catheter to drain their bladder when it fills and thereby undertake regular intermittent self-catheterisation (ISC). Intermittent catheterisation involves the introduction of a catheter into the bladder and its immediate removal when drainage stops, a process which needs to be repeated four to six times a day (Holroyd, 2018). The experience of performing ISC, while straightforward for some, can be both difficult and painful for others (Guinet-Lacoste et al, 2016; Rognoni and Tarricone, 2017).

Nurses and nursing leaders continue to be overwhelmed by increasing challenges as the call to demonstrate higher levels of resilience gains momentum. And yet nurses continue to be faced with unparalleled levels of adversity, leading to a loss of hope, with many choosing to leave the profession rather than continue to be exposed to unyielding levels of stress that have the potential to threaten the survival of the profession itself. With this in mind, this paper focuses on the importance of nurses working collaboratively through the process of coaching, a construct gaining momentum as the profession seeks to expand and facilitate new ways of working in order to develop both current and future nursing leaders and, in so doing, not only strengthen the voice of nursing, but also improve the way in which nurses practice.
It is estimated that 1.5 million children and young people (Paediatric Continence Forum [PCF], 2024), that is one in 12, across the UK battle debilitating, misunderstood and sometimes complex bowel or bladder conditions, including bedwetting, daytime wetting, chronic constipation and soiling.
This is a far bigger issue than many might think. Stigma around continence issues means that they are not talked about as much as other health conditions, and some people even delay seeking professional help because of embarrassment, or because they simply do not know what is wrong.
Chronic kidney disease is an ongoing decline of renal function which may progress quite rapidly or develop slowly over many years. Once diagnosed, patients are likely to become increasingly frequent attenders within general practice. This article provides an overview of the disease process and the multifaceted care needs of this specific patient group.
.png)
Have you heard about CLP Continence? It’s a dedicated platform, where we empower nurses specialising in continence care to become clinical leaders in their field. Our Clinical Leadership Programme is an educational resource designed to elevate your expertise and advance your career.
Find out about a recently launched guide for catheter users providing comprehensive information about the different types of catheters, their uses, and the latest innovations in technology.

Rectal cancer is common in the UK, affecting about 12,000 people each year. This article examines surgical treatment and likely subsequent problems with bowel function. It outlines how nurses can assist with simple interventions and what to do next if these do not work.

Continence is not a life-threatening condition but does affect an individual’s quality of life and the lives of their family and carers. This article explores the most common types of bladder and bowel problems and how to improve patient care. It looks at the prevalence of conditions, different types of continence issues, how they can affect quality of life and the complications that can occur when poorly managed.

Diagnosing and managing lower urinary tract infections (UTIs) in women aged 65 years and over is important to ensure their health and wellbeing. This article explores how to diagnose lower UTI, considering alternative diagnoses especially in older adults. It also looks at how to manage and treat uncomplicated lower UTI and provides guidance on recurrent UTI.

In the second of a two-part series, Ann Yates concentrates on the multiple causes/risks of faecal incontinence, the knowledge and skills required to complete a basic assessment and initiate conservative therapies, including the role of medication and pelvic floor rehabilitation, and also discusses management options for faecal incontinence.

This article is based on published research, together with the practical experience of healthcare professionals at the Complex Wound Clinic in North West London. The aim is to highlight the importance of considering skin tone when managing IAD.

Genitourinary syndrome of the menopause is an umbrella term to more accurately describe a range of vulvovaginal and lower urinary tract symptoms related predominately to low oestrogen levels. Here, Sue Thomas, advanced nurse practitioner, discusses the complications that can arise.
.jpg)
Faecal incontinence is the term describing the inability to control the bowels. This can include the uncontrolled passage of solid or liquid stool or of flatus (wind) through the anal canal. It is recognised as a symptom rather than diagnosis and is the result of complex interactions of many contributing factors. This series of two articles will look at this taboo condition, how it affects quality of life, highlight the anatomy and physiology which affects bowel control and then discuss conditions and contributing factors that make individuals prone to the symptoms of faecal incontinence.

A frequent side-effect of chronic coughing is urinary incontinence (UI) — mainly stress urinary incontinence. Although quite prevalent within this cohort of individuals, there seems to be little professional knowledge with regards to interventions to prevent or treat UI. This article looks at the causes of chronic coughing and how it impacts on UI.

Lynch syndrome is an inherited genetic condition and there could be over 175,000 people in the UK. About half of all people with Lynch syndrome develop colorectal cancer and it is also responsible for other cancers, including endometrial, gastric, small bowel, urothelial and brain cancers. This article outlines what Lynch syndrome is, how people can be screened and why testing is so important.
Overactive bladder syndrome is a little known chronic condition that affects both men and women. It can have a significant impact on an individual’s physical, psychological, social and financial quality of life. This article explores the assessment and conservative and pharmacological treatment options.

Bowel Cancer UK is the UK’s leading bowel cancer charity, determined to save lives and improve the quality of life of everyone affected by bowel cancer. Its vision is a future where nobody dies of the disease.

1 in 8 men will get prostate cancer, and some men experience urinary and bowel problems as a side effect of their treatment. A lack of public understanding of the condition, the stigma surrounding incontinence and the lack of facilities for men are damaging men’s physical and mental health.

Interstitial cystitis (IC) is a disease which, despite years of research, remains poorly understood. This article hopes to give healthcare professionals more knowledge of this complex disease so that they can facilitate earlier diagnosis and treatment, reducing the risk of misdiagnosis, which will ultimately improve outcomes and reduce the impact on the health and wellbeing of all those with this condition.

Many men are receiving androgen deprivation therapy for non-localised prostate cancer and side-effects of hormone therapy treatment may significantly impact quality of life. This editorial examines the seen and unseen side-effects of hormone therapy and support available from Prostate Cancer UK.

With influential organisations demonstrating a strong presence on social media, use of online social networking sites is gaining increasing momentum among healthcare professionals, including the nursing community. This editorial discusses the safe and professional use of social networking sites.
.jpg)
In this article, Marta Marchetti discusses the development of a unique, advanced nursing dual role in urology.

What does the future of digital hold for the clinical workforce? Liam Cahill explains what healthcare professionals currently do, what they want to be able to do, and what will inevitably help them to do this.

Early diagnosis of bowel cancer is key to saving lives. It is the UK’s second biggest cancer killer with more than 16,500 deaths from the disease every year — one every 30 minutes. Yet, it is treatable and curable if detected early. Here, Gerard McMahon discusses the quantitative faecal immunochemical test if it has the potential to transform bowel cancer diagnosis.

Many people across the UK live with poor bowel health, suffering with chronic constipation and/or faecal incontinence, which can be debilitating and prevent those suffering from enjoying their best life possible. Here, Jen Lodge and Angela Crossland discuss transanal irrigation and the importance of evidence-based practice.

Here, Carole Young, professional nurse advocate, independent nurse consultant and associate lecturer, Anglia Ruskin University, reflects on the impact of the pandemic on specialist nurses in the last two years and considers what is needed next in terms of support and recovery of self and service.

Wendy Osborne, clinical governance lead at Coloplast UK, describes a recent event highlighting why it is essential for everyone with a stoma to have equitable access to high quality care and specialist advice and gave people with a stoma an opportunity to have their voices heard.

Scott Newman, a specialist nurse from Prostate Cancer UK, discusses why an accurate and reliable test to detect prostate cancer is needed.

Many healthcare professionals recommend absorbent pads for men with urinary incontinence. To provide a high level of holistic care, patients should be made aware of all suitable management options appropriate for them to be empowered to manage their bladder accordingly.

Indwelling urinary catheters are one of the most commonly used devices in health care. When they are left in situ for longer than necessary, the person is put at risk of complications while waiting for an appointment to have it removed. This article discusses the transition from hospital to a community-based nurse-led TWOC service and its benefits.

Zena Aldridge delivers a call to action to all those who are working and interested in the field of dementia and continence.

Bowel Cancer UK is the UK’s leading bowel cancer charity, determined to save lives and improve the quality of life of everyone affected by bowel cancer. Its vision is a future where nobody dies of the disease.

Faecal incontinence has a huge impact on patient quality of life. Despite this, it can take many years for patients to open up and admit to friends, relatives or healthcare professionals that they are suffering. This article reviews the latest research and highlights the need for sensitive and supportive consultations with this patient group.

During the pandemic, urgent referrals for suspected urological cancer in England dropped by 56,000 from April 2020 to December 2021, resulting in approximately 13,500 fewer men in England starting treatment for prostate cancer compared to the same period in 2019. In this article, Prostate Cancer UK explains why this is a worrying statistic.

Childhood continence problems are common. One in 12 children are affected by a bowel or bladder problem: that’s around three children in every primary school class. Here, Jackie Fuidge discusses what ERIC, the Children’s Bowel & Bladder Charity, has to offer.

clinical nurse specialist for bladder and bowel; chair, RCN Bladder & Bowel Forum; Queen’s Nurse

Eighty percent of men diagnosed with prostate cancer will end up with erectile dysfunction after treatment (Downing et al, 2019). Yet, talking about sex, treating erectile dysfunction, and meeting the man’s needs after treatment is often lower down on the healthcare professional’s agenda. Prostate Cancer UK found that sex and erectile dysfunction is the biggest unmet need for men with prostate cancer.

Covid-19 has rapidly altered service provision and specialist professionals working across different geographical areas have not yet had sufficient opportunity to come together in person and process what these changes mean for their practice and patients. This upheaval has, of course, affected everyone whose work touches on bladder and bowel issues.

This article, the second in a two-part series, discusses conservative treatments for urinary incontinence and pelvic organ prolapse, which should be considered as first-line options where possible.
.png)
Last year, as part of continence awareness week, University Hospitals of Leicester NHS Trusts adult continence team launched their ‘taste the difference challenge’. The team worked collaboratively with ward staff and housekeepers in Leicester’s Hospitals, to promote and offer decaffeinated tea and coffee to inpatients across the trust.

In this article, the first in a new regional series, Ann Yates examines how the initial NHS was set up, how devolution in Wales has changed how services in Wales are commissioned and how this has impacted on continence/bladder/bowel care in Wales.

Fluid balance monitoring in health and social care has been a routine monitoring tool carried out by nursing staff for many decades. This article looks at the variety in terminology and practice, discusses the importance of maintaining accurate monitoring, and the essential components of a useful monitoring tool. It also identifies some of the challenges faced in maintaining effective monitoring of fluid balance with suggestions for improving practice.

Indwelling urinary catheters remain one of the most used clinically invasive devices in the UK, with approximately 90,000 people living in community settings in England currently using long-term urinary catheters. Use of a catheter valve system may improve the chance of normal bladder function resuming following the removal of the catheter. This article explores some of the clinical evidence supporting the use of catheter valves and advice on best practice.
Urinary tract infections are the second most common infection after chest infections. Here, The Urology Foundation highlights how they champion the nurses working in urology who go above and beyond to improve their patients’ treatment and care, and how one nurse transformed practice in the field of urinary catheters.

Like many organisations and charities, the Covid-19 pandemic hastened a rapid period of adaptation and diversification at ERIC, The Children’s Bowel and Bladder Charity. Here, Alina Lynden, ERIC’s communications manager explains how the charity has risen to the challenge.

Pelvic organ prolapse and urinary incontinence are common problems experienced by women of all ages. This article, the first in a two-part series, discusses the signs and symptoms of pelvic organ prolapse and urinary incontinence.

Meg Burgess is a Specialist Nurse at Prostate Cancer UK, providing support and information to anyone diagnosed with or concerned about a prostate problem via telephone, email, and live chat services. In this article, Meg talks about why fatigue support is needed, how it is delivered at Prostate Cancer UK, and the small changes men can make to help reduce the impact of fatigue on their quality of life.

The fourth and final part of the continence clinical skills series identifies how continence problems, which may not have responded to conservative treatment/ interventions, can be managed by the appropriate use of equipment/devices and products. The range available is vast and variable and some are more suitable to specific conditions than others. Healthcare professionals need to understand how they work to offer the best solution for individuals and their lifestyle. Products include, for example, commodes, urinals, sheaths, catheters, anal irrigation and pad products. This article specifically looks at equipment/devices and products for urinary retention, e.g. catheters; urinary incontinence, e.g. sheaths, pubic pressure devices; and faecal incontinence, e.g. anal plugs, transanal irrigation (TAI) and pad products.

Urinary and faecal incontinence are common in the older population, yet incontinence is not a normal part of ageing. Dementia can impact upon a person’s ability to remain continent, yet incontinence is unlikely to be a symptom of dementia until the latter stages of disease progression. There is a misconception that nothing can be done if a person with dementia experiences episodes of incontinence. However, many people with dementia often experience functional incontinence caused by immobility, communication difficulties, disorientation, or the inability to find the toilet, which can all be alleviated if the right support and advice is available.
.jpg)
Rectal interventions are a fundamental part of nursing care across all settings aimed at establishing whether effective bowel emptying is taking place. It is prudent for all clinicians to review their current knowledge and practice to ensure that they are following the latest evidence-based guidance for safe and effective practice.

The third part of the continence clinical skills series identifies what conservative therapies and treatments are available to treat bladder and/or bowel dysfunction. This includes a range of treatment options which can be provided by practitioners/clinicians from a multitude of healthcare professional disciplines. It highlights simple interventions, such as lifestyle changes, i.e. from diet, fluid, smoking and weight loss advice, up to the more complicated treatment options such as pelvic floor rehabilitation, bladder retraining and use of medication.

Functional constipation is a significant problem in childhood, not only due to its prevalence, but also the impact that it has on quality of life for the affected child and their families. However, the symptoms are often unrecognised by both parents and healthcare professionals, perpetuating the problem.

As Specialist Nurses at Prostate Cancer UK, we provide information and support to thousands of men living with and concerned about prostate cancer.

The second part of a continence clinical skills series looks at the requirements to undertake a basic continence assessment for bladder and/or bowel dysfunction. Assessment is the first step in identifying the type of continence issue an individual may suffer from. It should identify, for example, key elements of underlying medical history, presenting symptoms and duration of problem, medications, allergies, mobility and cognitive ability. This assessment should be supported by investigations, e.g. bladder and/or bowel diary, fluid/dietary intake, urinalysis, assessment of any post-void residual urine and pelvic floor/rectal examinations (if competent in skill).

Catching it early: recognising prostate cancer in asymptomatic men
By: Improving care team, Prostate Cancer UK
Many men with prostate cancer do not experience symptoms until the disease has spread. This means that they risk being diagnosed too late when the cancer is incurable. Nurses are in a unique position, as they are ideally placed to recognise men at higher risk of prostate cancer.

Continence is not a life-threatening condition but does affect patient quality of life. The first part in this new continence clinical skills series explores continence issues and how to improve patient care. It looks at the prevalence of the condition, different types of continence issues, how they can affect quality of life and the complications that can occur when poorly managed.
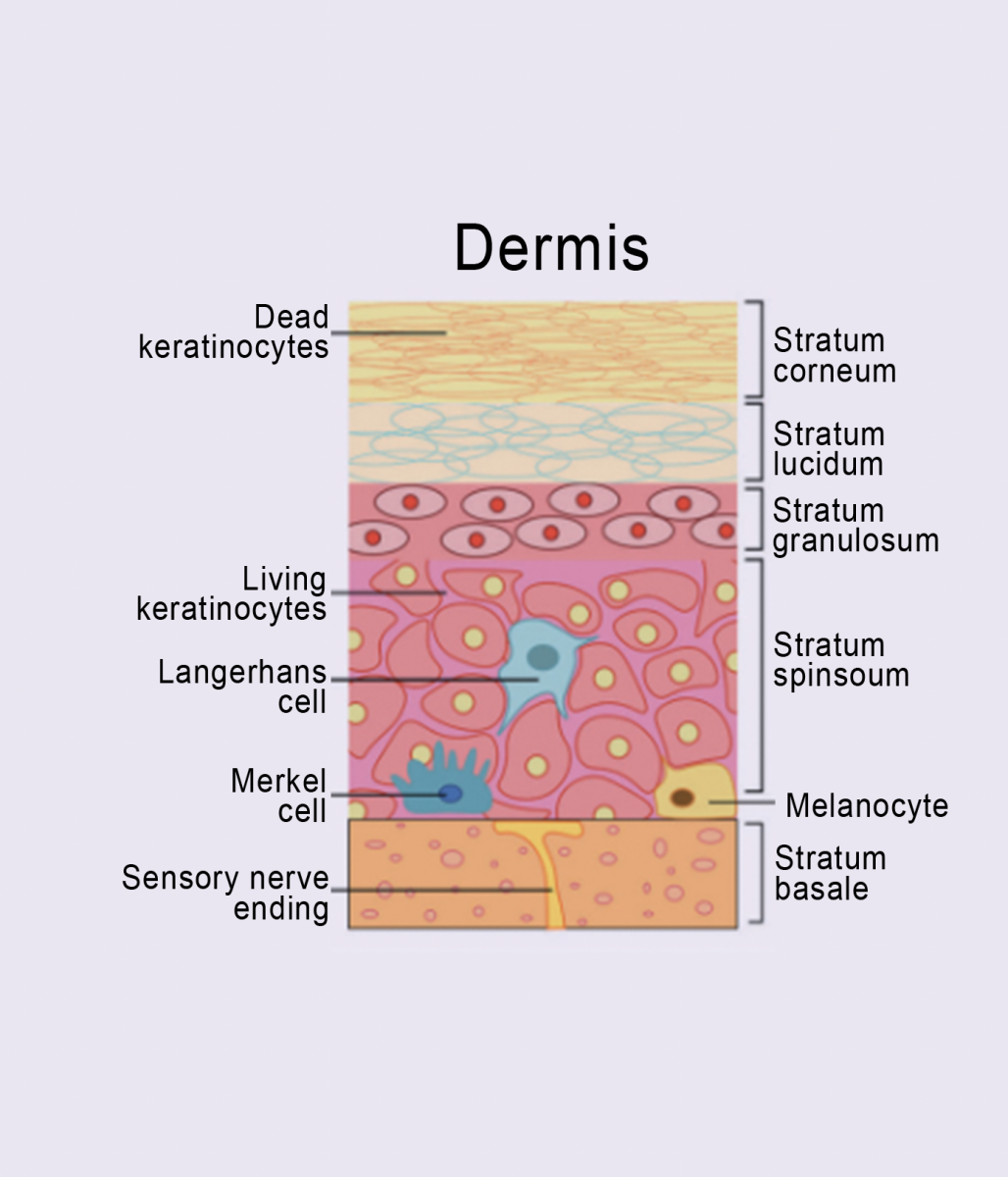
Moisture-associated skin damage (MASD) is the damage occurring in response to prolonged skin exposure to moisture and incontinence-associated dermatitis (IAD) is the most recognised form of MASD. IAD impacts physical, psychological and social health and is challenging for healthcare professionals to accurately identify and effectively treat.

Over 20 million people suffer from some form of bladder or bowel issue in the UK (NHS England, 2018). Continece problems can be caused by a number of factors, particularly vaginal childbirth (Barrie, 2015). This article discusses the recently published guidance document from the Royal Collage of Nursing (RCN), Bladder and bowel care in childbirth (RCN, 2021) - providing information for women throughout pregnancy, labour and into the postnatal period.

Urological conditions will affect one in two people during the course of their lifetime, yet they remain shrouded in secrecy and silence. This article highlights the work of The Urology Foundation, the only medical charity which works across the breadth of all urology diseases and is dedicated to improving the nation’s urological health.
.jpg)
It is easy to say you are holding an awareness month, but let’s consider the why, what and how.

This article examines the guidance available for school leaders, proprietors, governors, staff and practitioners to help them better support children and young people with bladder and bowel issues as they return to school.

Urinary incontinence is prevalent in men, with 61% of the general population of men experiencing lower urinary tract symptoms. These symptoms present as problems with voiding, storage or post-micturition of urine. Even after assessment and treatment, some men are still left with urinary incontinence, which is normally managed or contained by either pad products or urinary catheters (if clinically indicated). However, there is a vast range of alternative devices for containment. This article reviews some of the alternative devices that are available, namely sheaths, body worn urinals and penile compression clamps. It discusses the merits and disadvantages of each device and advises when they should or should not be used.

It is estimated that one in 12 children and young people in the UK suffer with a wetting or soiling problem, which can have a devastating impact on their family life, social life and self-esteem. Left untreated, bladder and bowel problems can cause serious health complications, but with the right treatment and support most children can overcome their problem or learn to manage it. This article outlines what ERIC, The Children’s Bowel & Bladder Charity, can do to help.

‘Urinary incontinence is among the most common paediatric problems and it is commonly assumed to resolve with age. Consequently, parents and clinicians often adopt a ‘wait and see’ approach. A significant proportion of children, however, continue to suffer from persistent urinary incontinence into adolescence. This article describes the development of a smartphone app to aid adherence to bladder training in young people with urinary incontinence.

Indwelling urinary catheters are still one of the most commonly used invasive devices in health care, with recognised significant risk factors, including catheter-associated urinary tract infection (CaUTI) and sepsis. Timely and successful removal of the catheter often falls to the responsibility of community nurses. There has been much debate about the optimum timing and circumstances for a successful trial without catheter (TWOC). This article looks at best practice guidelines and relevant clinical evidence to support healthcare professionals in making choices around TWOC procedures.

World Continence Week (WCW), taking place from 21–27 June, is an annual health campaign run by the World Federation for Incontinence and Pelvic Problems (WFIPP). The campaign highlights the impact that urinary incontinence can have on people’s lives and encourages sufferers to seek help to improve their quality of life.

Current Covid restrictions have forced many healthcare professionals to embrace technology and work in very different ways. Indeed, the traditional telephone has allowed the Newcastle continence service to provide a service to patients referred with all types of urinary incontinence. But, is it even possible to assess someone’s continence and devise a treatment plan over the telephone?
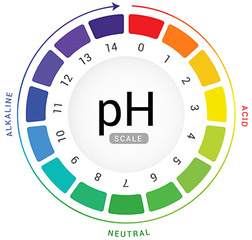
The maintenance of skin pH is essential if it is to provide a barrier to the outside world. This article examines how skin pH is maintained normally, what can disrupt it and the consequences of change. Finally, best practice guidance on restoring and maintaining a healthy skin pH and barrier function is provided.
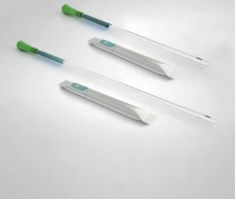
As a clinician, it is important that you are aware of the latest products and innovations that have the potential to improve outcomes for you and your patients. Each month, UCCT will highlight a product that is new, improved or innovative in order to keep you up to date.
Here, we present GentleCath™ Glide, a hydrophilic urinary catheter that uses FeelClean™ Technology to facilitate smooth, fast and convenient intermittent catheterisation.

As a clinician, it is important that you are aware of the latest products and innovations that have the potential to improve outcomes for you and your patients. Each month, UCCT will highlight a product that is new, improved or innovative in order to keep you up to date.
Here, we present PROSHIELD◊ Skin Care, which is formulated for the prevention and management of Incontinence-associated dermatitis on both intact and injured skin.

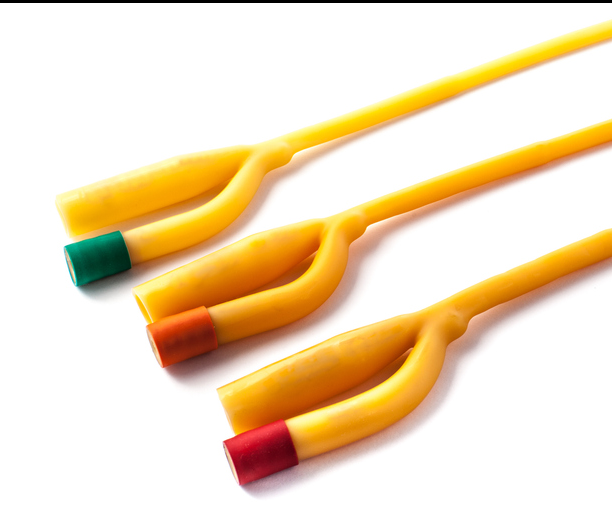
Patients in the community often have a long-term catheter in place and so their management inevitably becomes the responsibility of community nurses. As urinary incontinence can cause patients discomfort and have a negative impact on their day-to-day life, it is important that healthcare professionals understand the reasons for catheterisation and are aware of the different treatment options available, such as urethral and suprapubic, in order to provide patients with the most suitable device according to their needs and lifestyle. This paper explores the issues involved with indwelling catheterisation and looks at one new product range that aims to promote patient comfort and reduce associated risks.

Here, Sharon Holroyd, lead CNS, Calderdale Bladder and Bowel Service; chairperson, Yorkshire ACA, defines stress urinary incontinence and the treatment options available, and reviews the evidence to support pelvic floor exercises as an effective rehabilitation for patients with symptoms of stress urinary incontinence.
Nocturia is a common lower urinary tract symptom that mainly affects older people. Nocturia causes excess urination at night and, because of associated night-time rising, can also result in falls and fractures. Nocturia has a range of presentations, therefore it is vital that nurses understand how to assess the condition accurately to provide appropriate treatment. This article examines the effective assessment of nocturia, as well as detailing the various lifestyle treatment options that can be used, such as a targeted reduction of fluid intake, weight loss and altered medication profiles. Medication and surgical options should only be used following a trial of lifestyle interventions.
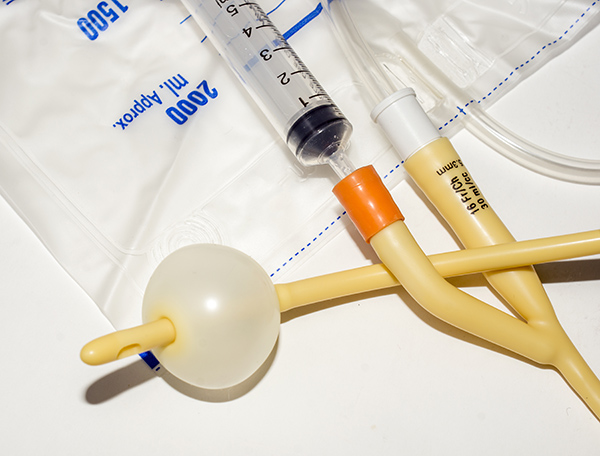
Indwelling urinary catheters remain one of the most commonly used clinically invasive devices across the NHS and social care in the UK. The problems associated with the prolonged use of catheters are widely referenced. Healthcare-acquired infections (HCAIs) currently result in 5,000 preventable deaths a year, with 20% of all HCAIs associated with the urinary tract. Many staff have learned catheterisation techniques in their early careers, with no need for a formal review of skills and knowledge. This has perhaps contributed to some historical and now outdated tasks still being performed. The evidence for best practice when managing indwelling catheters is reflected in national and international guidelines, which have recently undergone a complete overhaul. This article explores common practices and best practice evidence to assist with safe and effective management of these essential but often risky devices.

There are a variety of reasons as to why a patient may require an indwelling catheter, however, these are seldom documented or communicated across healthcare services (Codd, 2013). Thus, shortterm catheters are at risk of becoming long-term catheters in the absence of clear documentation and forward planning. The risk of infection increases the longer a urinary catheter remains in situ. This article explores the guidance available to support appropriate urinary catheter use, catheter management, documentation, forward planning and patient education for effective catheter care. How this can be implemented to support appropriate removal of urinary catheters or ongoing care for long-term urinary catheter use for patients across the primary and secondary care services is also discussed.

This two-part article aims to help healthcare professionals understand constipation; the possible causes, and the anatomical and functional problems. In the first part, the author explained anatomy and physiology of the lower gastrointestinal tract, what are normal bowel motions, frequency and variation, which includes the Bristol Stool Chart to view the types of bowel motions sufferers may often experience. Here, the focus is on conservative treatment interventions for constipation, exploring the four ‘Fs’ acronym (Rex, 2013): fibre (in diet); fluids (those best for health reasons); fitness (‘if you do not move, it will not move’); and finally feet, which relates to the best sitting position to help achieve bowel evacuation successfully.

Bowel dysfunction is a common problem for adults and children, and yet many people do not seek help and when they do it is not up to standard. Unmanaged symptoms impact on the health of the patient, both physically and mentally, and add extra cost to the NHS. This article, by a clinical nurse specialist working with people suffering from bladder and bowel dysfunctions, will help healthcare professionals understand the possible causes of anatomical and functional bowel problems, especially constipation, and the conservative treatment interventions. This First article in a two-part series, explains anatomy and physiology of the lower gastrointestinal tract, what constitutes a normal bowel habit, frequency and variation. The second will focus on the causes of constipation, which are often misunderstood and misdiagnosed, and how they can be assessed and managed, as well as treatment options available.

As a clinician, it is important that you are aware of the latest products and innovations that have the potential to improve outcomes for you and your patients. Each month, UCCT will highlight a product that is new, improved or innovative in order to keep you up to date.
Here, we present MoliCare® Premium Elastic, a new generation slip which is designed to ease application while offering comfort and security for the wearer.
The National Catheter Education Programme is a Health Education England-funded initiative to improve the care of patients with catheters. Part of this initiative is the Secret Life of Catheters programme. This article highlights the need for improvement in catheter care and explains the development of this project, which aims to drive improvements across primary and secondary settings through the large-scale delivery of a multiprofessional educational programme in catheter care. The programme explores key dilemmas that district nurses, community nurses, healthcare assistants and doctors can encounter with catheters, and provides approaches to address them. By standardising the teaching of clinical concepts and practice strategies, it is hoped that variations in practice and pockets of misunderstanding can be eliminated.

Transanal irrigation has been acknowledged as a minimally invasive technique with proven clinical evidence of benefit, partciularly in patients with neurogenic bowel disorders. The severity of impairment in patients with neurogenic bowel disorders will depend on the level of spinal cord damage and may lead to a loss of the sense of needing to defecate, loss of control of the external sphincter, loss of muscle tone and contractility of the bowel / rectum, and disrupted transit time. Any transanal irrigation system chosen will require careful assessment of the patient's needs and preferences before treatment is initiated. There is also a need for ongoing support from a suitably experienced healthcare professional to ensure compliance and efficacy. Although the initially cost of transanal irrigation systems may seem expensive, when compared to the long-term cost of other treatments, repeated tests and hospital admissions, they represent a more cost-effective long-term option.
The effect of drugs on mental and physical health are well documented. However, these consequences do not necessarily prevent people using them either recreationally or more regularly, with some becoming addicted to their drug or drugs of choice. It is estimated that in 2016/17, around one in 12 (8.5%) adults aged 16 to 59 in England and Wales had taken an illicit drug in the last year (NHS Digital, 2018). Ketamine has become increasingly popular, especially among younger users, as it is cheap and mistakenly seen as a ‘safe’, non-addictive drug. However, the reality is that even recreational use may have serious consequences. The effect on the urinary system can be devastating, with users experiencing anything from frequency and cystitis-like symptoms, to extreme debilitating pain from the inflamed and shrunken bladder, resulting in cystectomy and urinary diversion, and, if the kidneys are affected, renal failure and dialysis.

Urinary incontinence (UI) has been associated with chronic respiratory symptoms, which impact on patient quality of life (da Silva Paes et al, 2016). Chronic respiratory symptoms, such as coughing, wheezing, and dyspnoea, and patients with chronic chest conditions, such as asthma, bronchitis or chronic obstructive pulmonary disease (COPD), are associated with increased occurrence of UI. Women with respiratory symptoms have more severe symptoms and are more likely to have stress urinary leakage than those without. This paper provides an overview of asthma, and highlights the importance of community nurses not only addressing issues associated with respiratory diseases, such as ensuring that there is a personalised asthma action plan (PAAP) in place for those with asthma, but also assessing urinary incontinence to evaluate occurrence and decide upon measures that can be taken to prevent or lessen any leakage.

Kate Upton, registered adult nurse and fellow of the Higher Education Academy; representative for Nursing Professions on the Crisis, Disaster and Trauma Psychology Section of the British Psychological Society; independent nursing/medical tutor and medical writer; PhD student at the University of Birmingham

As a clinician, it is important that you are aware of the latest products and innovations that have the potential to improve outcomes for you and your patients. Each month, UCCT will highlight a product that is new, improved or innovative in order to keep you up to date.
Here, we present the Prosys® SensaCath® intermittent catheter range, which has been developed to enhance the patient experience during intermittent self-catheterisation.

Catheterisation has improved continence and reduced associated urinary tract problems. Intermittent catheterisation has been shown to be acceptable for all ages, including the elderly. The role of the nurse is important in teaching and supporting patients using clean intermittent catheterisation (CIC) to ensure confidence and adherence with the procedure. Some patients with indwelling catheters may experience poor body image and negative sexual self-esteem.

Urinary tract infection (UTI) is an important cause of morbidity and mortality in the healthcare setting, accounting for 19% of all nosocomial infections (Loveday et al, 2014).
It is estimated that 43–56% of these are catheter-associated urinary tract infections (CAUTI) (Loveday et al, 2014).
If inadequately treated, CAUTI may progress to bacteraemia and consequent urosepsis syndrome, multiplying the risk of mortality and extending hospital stay (Centers for Disease Control and Prevention, 2009).

Belinda Campbell started using a single-use urinary catheter in 2011. Although she did not have a proper diagnosis, she was told that her bladder and sphincter muscles did not work and that the connection between the brain and the bladder was not as it should be. Here, we ask Belinda about her journey and the support she has received in learning how to self-catheterise and coming to terms with a lifelong condition.

Kate Upton describes compassion fatigue, an increasingly reported form of stress associated with the demands of nursing in the current NHS, and questions what can be done to overcome it.

Over one million indwelling urinary catheters are inserted every year in the UK; this equates to between 12 and 24% of hospital patients having an indwelling catheter at some point during their inpatient stay (Feneley et al, 2015).
The use of indwelling urinary catheters in the care sector can be higher (Royal College of Physicians, 2004; Loveday et al, 2015).
Nurses should be familiar with best practice and understand the advantages and disadvantages of using indwelling urinary catheters in the urethral and suprapubic sites.
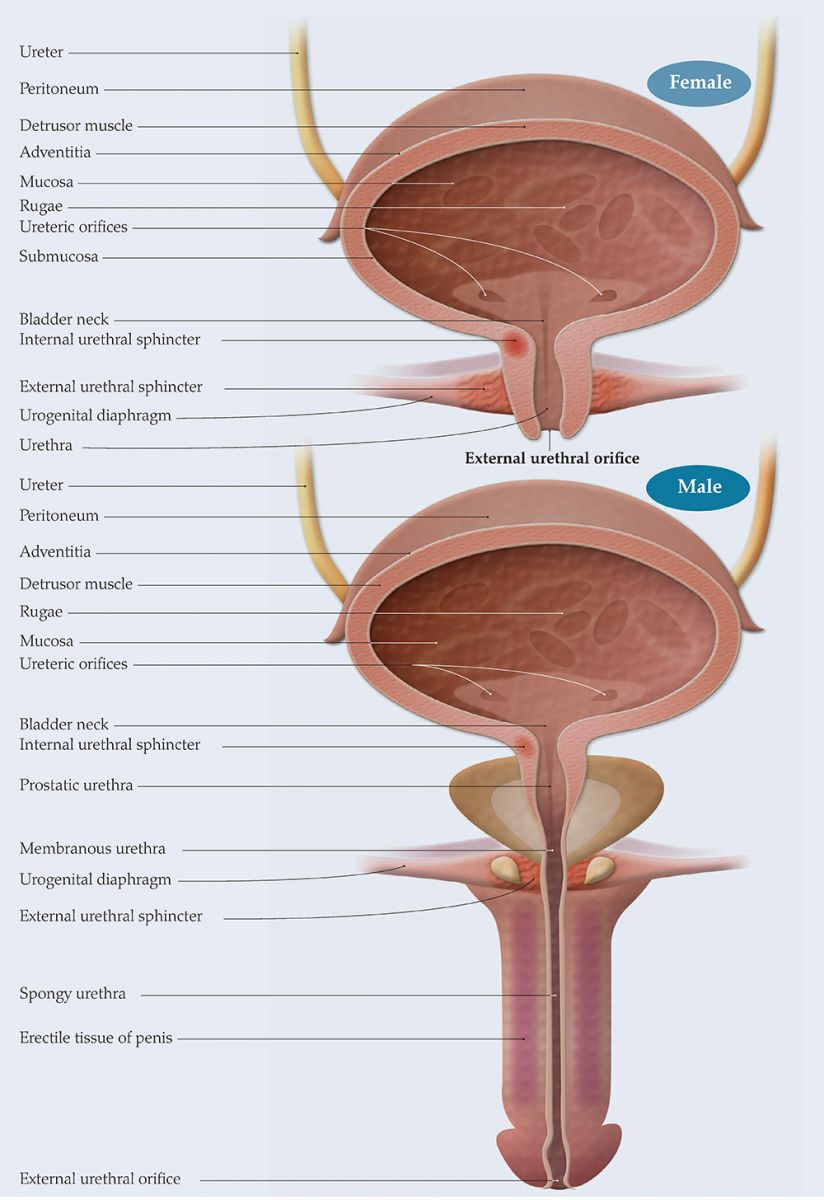
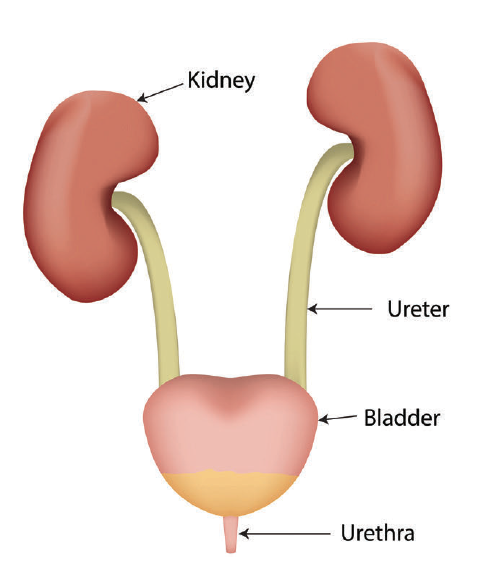
Passing urine is something most of us do not give a thought about, as it is part of everyday lives. However, it is a more complex process than is apparent, as all elements of the urinary tract need to be functioning and working together, and the three micturition centres in the body, which control filling and emptying of the bladder via the autonomic and somatic nervous systems, also need to work in harmony to urinate successfully. Here, Rachel Leaver, lecturer practitioner, urological nursing, UCLH and London South Bank University, UCLH NHS Foundation Trust, provides an overview of the male and female urinary tracts.

Continence is an important and common problem and so nurses have a responsibility to be able to screen for and perform a basic assessment of incontinence.
Resolution of continence issues is possible for many with the right care and advice.
Primary care nurses need the education and training to be able to offer advice and treatment to help meet people's continence needs and to know when to refer on to specialist services.

If a patient cannot empty their bladder completely, intermittent self-catheterisation (ISC) may be an acceptable treatment option.
Learning ISC can be daunting for patients and unless taught properly and the patient is given time to learn at their own pace, compliance may be a problem (Logan et al, 2008).
There are a huge variety of catheters available for ISC and each patient should be assessed individually to find out which option best suits their needs.

Patricia McDermott explains how the ACA is setting the standard for excellence and innovation in continence care today.

Jane Brocksom explains how BAUN has developed into the vibrant organisation it is today and the opportunities it offers to the profession.

Writing for publication is now unavoidable for healthcare professionals who want to progress their career. However, it can feel like a daunting process on top of the demands of the day job and home life. This first part of our writing for publication series, provides guidance on what you need to do before you even begin to write.

Catheters have been around for thousands of years, but the basic principles have not changed, so here we ask - Is it time to take a fresh look at catheter care and could we do better?