Nocturia is a widespread condition and one of the most significant lower urinary tract symptoms (LUTS) (Oelke et al, 2017). In the past, nocturia was defined by the International Continence Society as: ‘The interruption of sleep one or more times to void’ (Van Kerrebroeck et al, 2002). However, this was revised in 2017, with the accepted definition being changed to: ‘Waking to pass urine during the main sleep period’ (Hashim et al, 2019).
Nocturia is a complex, bothersome symptom that is connected with a significant decline in patients’ health status. This can negatively affect patients’ quality of life, causing sleep deprivation and falls, and increasing morbidity and mortality (Oelke et al, 2017). The prevalence of nocturia is similar in men and women and the condition affects 28–93% of people aged 40 years or older (Oelke et al, 2017). However, prevalence increases with (growths associated with cancer), anxiety disorders and medicines such as diuretics
- Increased fluid intake
- Increased diuresis: this can be subdivided into:
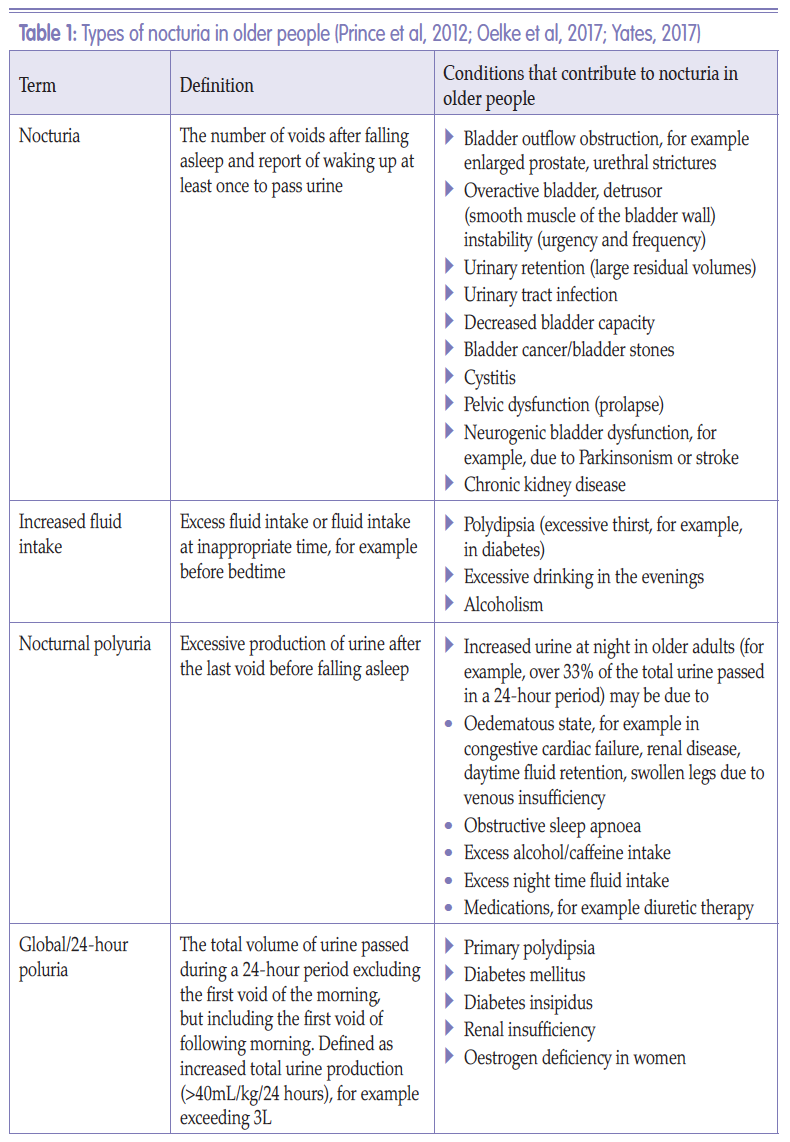
Conditions that contribute to the different categories of nocturia in older people are outlined in Table 1.
Nocturia is a complex, bothersome symptom that is connected with a significant decline in patients’ health status. This can negatively affect patients’ quality of life, causing sleep deprivation and falls, and increasing morbidity and mortality (Oelke et al, 2017). The prevalence of nocturia is similar in men and women and the condition affects 28–93% of people aged 40 years or older (Oelke et al, 2017). However, prevalence increases with (growths associated with cancer), anxiety disorders and medicines such as diuretics
- Increased fluid intake
- Increased diuresis: this can be subdivided into:
~ Global polyuria (continually raised bladder output)
~ Nocturnal polyuria.
Conditions that contribute to the different categories of nocturia in older people are outlined in Table 1.
QUALITY OF LIFE
The consequences of nocturia are varied and numerous. The condition is associated with an increased incidence of falls and fractures – especially hip fractures – and an increased fear of falling (Varilla et al, 2011). Falling is due to elderly people getting out of bed in the dark to walk to the bathroom to void. As patients’ sleep is disturbed and fragmented due to the need to void at night, they can become drowsy during the day. This can increase fatigue and reduce energy levels; impair balance, perception, concentration and memory; lower mood; and cause depression (Varilla et al, 2011). In turn, this can result in complications associated with immobility and debility, such as, pressure ulceration, malnutrition and increased risk of infection.The impact of nocturia on quality of life is comparable to the effects of other conditions, such as gout, hypertension, diabetes and angina. It also affects an individual’s perception of their age (i.e. people with nocturia feel older), as well as contributing to obesity and higher rates of death in patients with coronary heart disease. Nocturia can also lead to relationship disturbances or breakdown and increased admission to care homes (Varilla et al, 2011).
'The impact of nocturia on quality of life is comparable to the effects of other conditions, such as gout, hypertension, diabetes and angina. It also affects an individual’s perception of their age... '
ASSESSMENT OF NOCTURIA IN OLDER PEOPLE
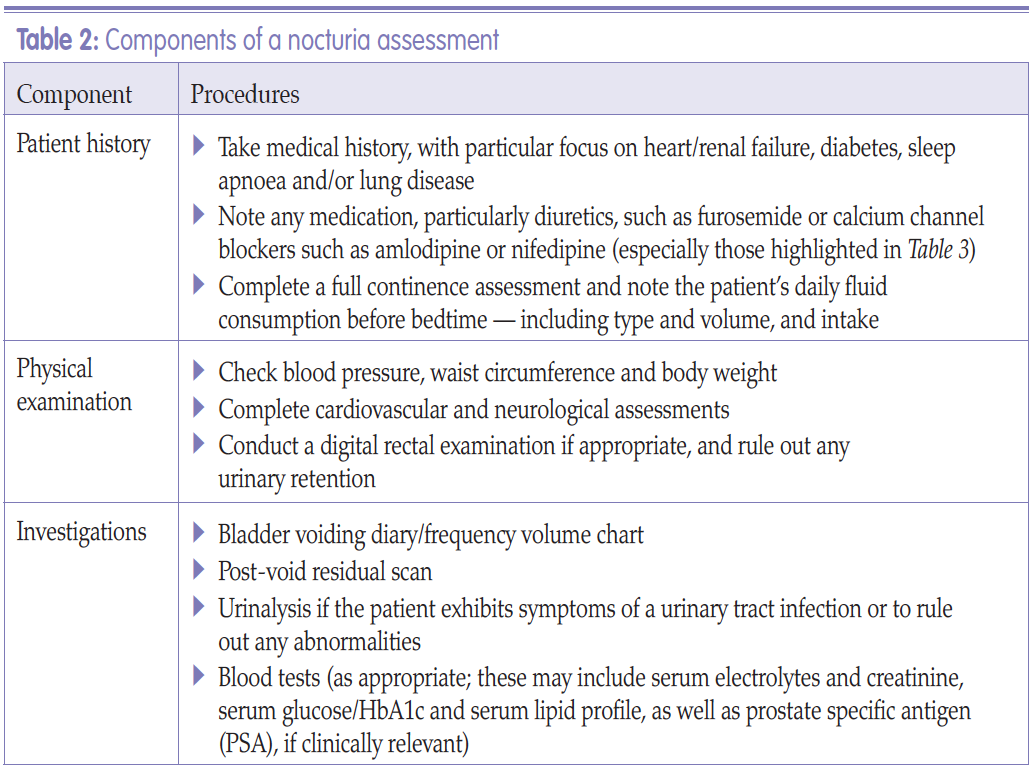
It is vital that healthcare professionals understand the complexities of nocturia and how different types of nocturia present before any treatment options are considered. This should be done by undertaking a thorough holistic assessment as outlined in Table 2. It is important that the nurse enquires as to the patient’s perception of their nocturia, and that the frequency of their night-time voiding is discussed.Fluid intake and use of charts
One of the most important aspects of nocturia assessment is to monitor the patient’s fluid consumption and record their urinary output via a frequency volume chart (FVC) or bladder diary, as well as understanding what types of fluid they are consuming and when.The amount and type of fluid an individual consumes during the day should be evaluated, as excessive daytime fluid consumption can be responsible for nocturia (Yates, 2017). Fluid intake at bedtime can also exacerbate nocturia, as can drinking caffeine-based drinks or alcohol. The use of an FVC or bladder diary is extremely useful for nurses when attempting to identify nocturia. The FVC or bladder diary can distinguish between different types of nocturia - for example, an excessive amount of fluid voided over a 24-hour period might indicate global polyuria — and should be completed for three days.
Even a basic FVC can be used to record the patient’s maximum bladder capacity, voiding times and how these are divided between night and day, voided volumes, and episodes of nocturia, as well as approximating when the patient falls asleep (Figure 1).
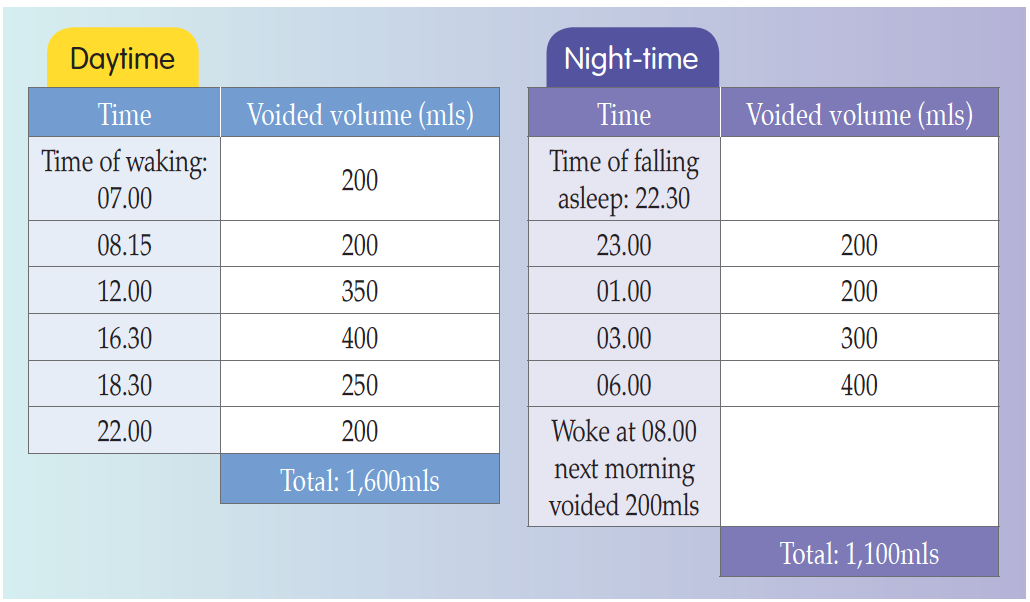 Figure 1.
Figure 1.Example of a frequency volume chart (FVC) (Hashim et al, 2019).
In the example detailed in Figure 1, the patient has a maximum bladder capacity of 400mls, passes urine six times during the day and four times at night, with the total amount voided at night (1,100mls) amounting to over 33% of the total volume passed in 24-hour period (2,700mls). Thus, the nurse can postulate that the patient is experiencing nocturnal polyuria. This could be due to this patient’s oedematous state, which in turn may be caused by:
- Congestive cardiac failure
- Renal disease
- Daytime fluid retention
- Swollen legs due to venous insufficiency
- Obstructive sleep apnoea
- Alcohol/caffeine input
- Excess night-time fluid intake
- Medication, such as diuretic therapy.
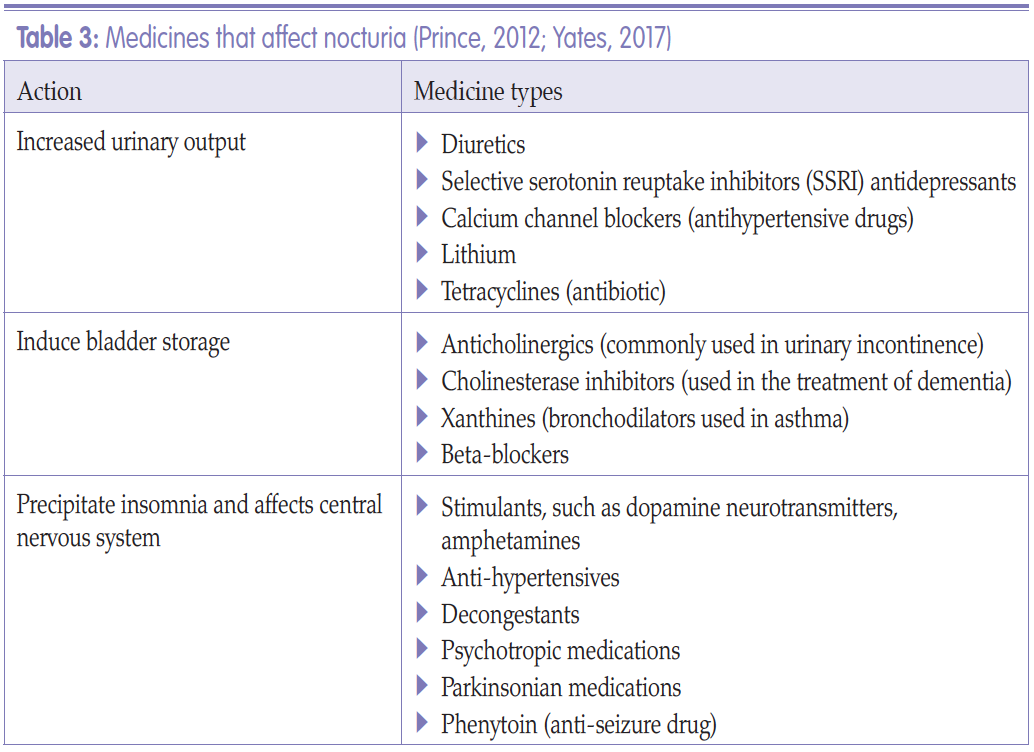
Medication
There are numerous medications that can affect nocturia, for example increasing the patient’s urinary output, inducing bladder storage issues, affecting sleep patterns or causing insomnia, or affecting the central nervous system (CNS). A summary of medications and their effects is shown in Table 3.
Physical examination
Before any treatment options are considered, comprehensive examination similar to that performed for the assessment of urinary incontinence should be undertaken. This should include (Yates, 2017):
- Examination of the cardiovascular and pulmonary systems: focusing on fluid overload and congestive cardiac failure
- Palpation of the abdomen: assessing for suprapubic masses and tenderness, and checking for bladder distension due to an abnormally high post void residual urine (a bladder scan is the preferred option for checking residual urine)
- Rectal examination: concentrating on faecal impaction, prostate size and pelvic floor. The bowel is said to be compliant, as the anal resting pressure (which is measured in centimetres of water) is low and does not increase when there is an increase in rectal content and it is full of faeces. This can impact on faecal loading and impaction within the rectum. The bowel compliance has no impact on the bowel closure mechanism. However, the pelvic floor and both internal and external sphincter muscles contribute to this closure mechanism. The internal anal sphincter is able to maintain tonic contraction for long periods of time, while external sphincter under voluntary control is fatigable. Damage to all parts can contribute to urinary/bowel problems (Emmanuel, 2004)
- Examination of lower extremities: assessing for the presence of pitting oedema (following pressure applied to a small area of skin, the indentation remains even following release of the pressure; due to excess fluid in the tissues)
- Neurological examination: looking for signs of either mental dysfunction, e.g dementia, or physical nerve damage, which can cause functional dysfunction, e.g. cerebrovascular accident, multiple sclerosis.
- Symptoms of obstruction, such as from an enlarged prostate, prolapse, urethral strictures or constipation
- Voiding hesitancy
- Weak urine stream, or incomplete emptying, or intermittency, i.e. when someone starts to void but it keeps stopping/starting for perhaps one of the reasons above. So instead of a good powerful flow it takes longer to empty bladder
- Urinary frequency, urgency or urinary incontinence (Johnson, 2017.
Box 1
NON-PHARMACOLOGICAL, BEHAVIOURAL AND LIFESTYLE NURSING INTERVENTIONS FOR NOCTURIA (OELKE ET AL, 2017; YATES, 2017)
- Address underlying cause of nocturia, for example, diabetes mellitus or prostate enlargement- Check individual’s medication profile for potential exacerbating drugs such as diuretics
- Recommend avoidance of caffeine/alcohol in the evening
- Recommend limiting excessive fluid/food intake 3–6 hours before bedtime
- Recommend limiting fluid intake to 2 litres per 24 hours if comorbidities allow
- Recommend reducing dietary salt intake
- Support weight loss if appropriate
- Recommend elevating legs in the evening
- Provide education on the use of compression stockings if appropriate
- Provide continuous positive airway pressure (CPAP) for obstructive sleep apnoea
- Change time of diuretics from evening to morning/afternoon
- Recommend emptying bladder before bedtime
- Provide education on pre-emptive voiding, i.e. emptying the bladder before the critical volume is reached before leakage. This is different for each individual but is a useful technique
- Optimisation of sleep environment, i.e. environment should be neither too hot nor too cold, as this prevents sleep; room should be dark and quiet (blackout curtains and ear plugs can be used); patients should be advised not to use screens (i.e. computers, phones, TV before bedtime) and to reduce non–sleep time in bed (Varilla et al, 2011)
- Ensure patient has barrier-free access to toilet - Provide or refer patient for pelvic floor rehabilitation/urge suppression techniques. Patients should be correctly instructed in pelvic floor exercises, which include suppression techniques, e.g. the knack (whereby you pull in pelvic floor muscles before sneezing, laughing, standing, etc), and 50% lift, whereby the individual is taught only to contract pelvic floor muscles for 50% of a lift, which means that they have the ability to hold on to contraction for longer, e.g. going up stairs, walking to toilet.
TREATMENT
Treatment for nocturia can involve non-pharmacological modalities, including behavioural therapies and lifestyle changes (Box 1); pharmacological interventions (Box 2); or surgical options. Surgical options are usually restricted to prostate surgery. However, nocturia is usually non-responsive to this type of surgery (Doorn and Bosch, 2012). Treatment options should start with lifestyle and behavioural changes, which should be attempted for up to three months before other treatments are tried (Oelke et al, 2017).Box 2
PHARMACOLOGICAL TREATMENT OF NOCTURIA
-Alpha-adrenergic blockers: anti-cholesterol drugs used to lower blood pressure; also used in nocturia; prescribed in men only- 5-alpha reductase inhibitors: drugs used to treat enlarged prostate glands; prescribed in men only
- Anticholinergics: care should be taken in prescribing in older people; the patient’s anticholinergic burden score (a method for assessing the potential effect on cognitive function of anticholinergic drugs) should be checked before administering these drugs
- Mirabegron: drug used to treat overactive bladder
- Topical oestrogen therapy: can be useful in treating urinary urgency; should be prescribed in women only
- Antidiuretic therapy should only be prescribed in people aged up to 65. Antidiuretic therapy helps to control the fluid balance in an individual’s body by reducing urination. Its effects are opposite to those of a diuretic. The major antidiuretics are antidiuretic hormone (ADH; also called vasopressin) and oxytocin
- Timed diuretic therapy: should not be administered at bedtime, but in the morning or afternoon
- Desmopressin: reduces the amount of urine produced by the kidneys; not licensed for people aged over 65; however, a new low-dose formula (Noqdirna; Ferring Pharmaceuticals) is available for idiopathic nocturnal polyuria, including people aged over 65.
CONCLUSION
Nocturia is a common multifaceted condition that commonly affects older people. It requires a comprehensive assessment and bespoke treatment options for each individual. It is vital that an FVC is completed and the patient’s medication reviewed as part of any assessment for nocturia. Treatment options should start with lifestyle and behavioural changes, which should be attempted before other treatments such as pharmacological interventions or surgery. Patients who do not respond to lifestyle interventions should be considered for specialist assessment.Key points
- Nocturia is a common condition particularly among older people.- Nocturia can have a significant negative effect on the individual’s quality of life and health status.
- Nocturia may signify the presence of an undiagnosed medical condition.
- A completed fluid volume chart is essential to understanding which type of nocturia is affecting the patient.
- Non-pharmacological, behavioural and lifestyle changes should be recommended initially.
References
Doorn BV, Bosch JLHR (2012) Nocturia in older men. Maturitas 71: 8–12
Emmanuel A (2004) Constipation. In: Norton C, Chelvanayagam S, eds. Bowel Continence Nursing. Beaconsfield, Beaconsfield Publishers Ltd
Hashim H, Blanker MH, Drake MJ, et al (2019) International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn 38(2): 499–508
Johnson TM (2017) Nocturia: clinical presentation, diagnosis, and treatment. Available online: www.uptodate.com/contents/nocturia-clinical-presentationdaignosis-and-treatment
Kujubu DA, Aboseif SR (2007) Evaluation of nocturia in the elderly. Perm J 11(1): 37–9
Oelke M, De Wachter S, Drake MJ, et al (2017) A practical approach to the management of nocturia. Int J Clin Pract 71: e13027
Prince D, Pedler K, Rashid P (2012) Nocturia — a guide to assessment and management. Aust Fam Physician 41(6): 399–402
Van Kerrebroeck P, Abrams P, Chaikin D, et al (2002) The standardisation of terminology in nocturia: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn 21(2): 179–83
Varilla V, Samala RV, Galindo D, Ciocon J (2011) Nocturia in the elderly: a wake-up call. Cleve Clin J Med 78(11): 757–64
Yates A (2017) Nocturia in older people living in residential care. Nurs Res Care 19(11): 616–18
Emmanuel A (2004) Constipation. In: Norton C, Chelvanayagam S, eds. Bowel Continence Nursing. Beaconsfield, Beaconsfield Publishers Ltd
Hashim H, Blanker MH, Drake MJ, et al (2019) International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn 38(2): 499–508
Johnson TM (2017) Nocturia: clinical presentation, diagnosis, and treatment. Available online: www.uptodate.com/contents/nocturia-clinical-presentationdaignosis-and-treatment
Kujubu DA, Aboseif SR (2007) Evaluation of nocturia in the elderly. Perm J 11(1): 37–9
Oelke M, De Wachter S, Drake MJ, et al (2017) A practical approach to the management of nocturia. Int J Clin Pract 71: e13027
Prince D, Pedler K, Rashid P (2012) Nocturia — a guide to assessment and management. Aust Fam Physician 41(6): 399–402
Van Kerrebroeck P, Abrams P, Chaikin D, et al (2002) The standardisation of terminology in nocturia: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn 21(2): 179–83
Varilla V, Samala RV, Galindo D, Ciocon J (2011) Nocturia in the elderly: a wake-up call. Cleve Clin J Med 78(11): 757–64
Yates A (2017) Nocturia in older people living in residential care. Nurs Res Care 19(11): 616–18


