References
Codd J (2013) Implementation of a patientheld urinary catheter passport to improve catheter management, by prompting for early removal and enhancing patient compliance. J Infect Prev 15(3): 99–9
Houghton M (2017) Urinary Catheter Care Guidelines. Southern Health NHS Foundation Trust. Available online: www.southernhealth.nhs.uk/_resources/assets/inline/full/0/70589.pdf
Jaeger M, Fox F, Cooney G, Robinson J (2017) A qualitative study exploiting the value of a catheter passport. Br J Nurs 28(15): 857–66
Kirmusaglu S, Yurdugul S, Metin A, Vehid S (2017) The effect of urinary catheters on microbial biofilm and catheter associated urinary tract infection. Urol J 14(2): 3028–34
Loveday HP, Wilson JA, Pratt RJ (2014) EPIC 3: national evidence-based guidelines for preventing healthcare associated infections in NHS hospitals in England. J Hosp Infect 86(Suppl 1):S1–S70
Mantle S (2015) Reducing HCAI — what the commissioner needs to know. NHS England, London. Available online: www.england.nhs.uk/wp-content/uploads/2015/04/09- amr-brim-reducing-hcai.pdf
National Institute for Health and Care Excellence (2006) Urinary incontinence: the management of urinary incontinence in women. Clinical guideline 40. NICE, London
National Institute for Health and Care Excellence (2014) Infection Prevention and Control Quality Standard [QS61]. NICE, London. Available online: www.nice.org.uk/guidance/qs61/chapter/qualitystatement4-urinary-catheters (accessed 20 May, 2018)
National Institute for Health and Care Excellence (2016) Healthcare associated infections. NICE, London. Available online: www.nice.org.uk/guidance/qs113 (accessed 4 May, 2018)
National Institute for Health and Care Excellence (2017) Healthcare-associated infections: Prevention and control in primary and community care. Clinical guidance 139. NICE, London. Available online: www.nice.org.uk/guidance/cg139/ifp/chapter/long-term-use-of-urinary-catheters (accessed 19 May, 2018)
Nursing and Midwifery Council (2015) The Code: Professional Standards of Practice and Behaviour for Nurses and Midwives. NMC, London
Pannell L, Tyrell-Price J (2017) Communication between primary and secondary care. Br J Hosp Med 78(8): 464–6
Pellowe C (2009) EPIC 2 infection prevention guidelines — best practice. Continence UK 3(3):28–33
Royal College of Nursing (2012) Catheter care. RCN, London
Royal College of Nursing (2016) Infection prevention and control commissioning toolkit — guidance and information for nursing and commissioning staff in England. 3rd edn. RCN, London
Shackley DC, Whytock C, Parry G, et al (2017) Variation in the prevalence of urinary catheters: a profile of national health service patients in England. BMJ Open 7(6): e013842
Simpson P (2017) Long-term urethral catheterisation: guidelines for community nurses. Br J Nurs 26(9 Suppl): S22–S26



 As said, comprehensive assessment is required before an indwelling catheter is inserted and the healthcare professional must have a clear rationale for its use. The patient should also be involved in their care and provided with both written and verbal information to ensure that they can make an informed choice (RCN, 2012). The reason for catheterisation needs to be discussed with the patient and consent gained before insertion (NICE, 2014).
As said, comprehensive assessment is required before an indwelling catheter is inserted and the healthcare professional must have a clear rationale for its use. The patient should also be involved in their care and provided with both written and verbal information to ensure that they can make an informed choice (RCN, 2012). The reason for catheterisation needs to be discussed with the patient and consent gained before insertion (NICE, 2014).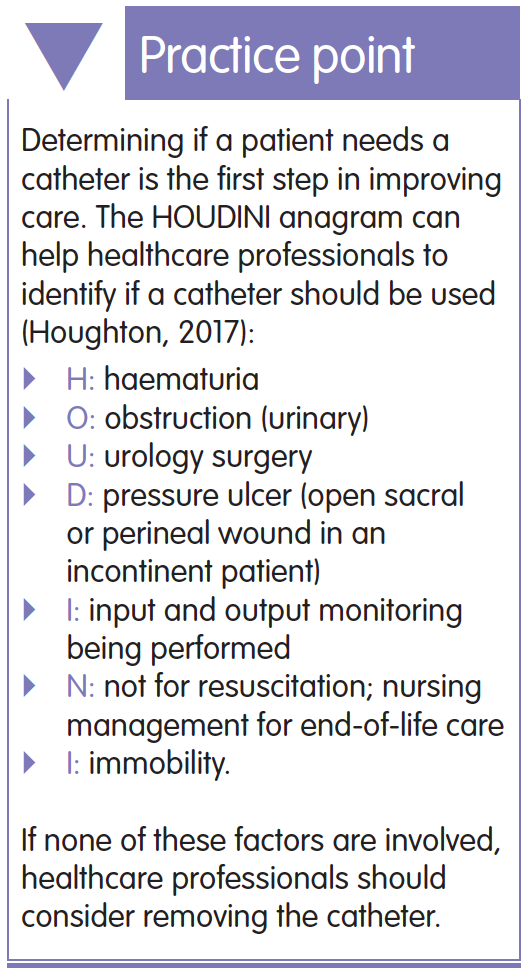
 Avoiding unnecessary urinary catheterisation prevents the risk of CAUTI. Healthcare professionals should therefore challenge the need for a urinary catheter and ensure that patient assessment is completed before carrying out the procedure. In circumstances where there is a clinical requirement for an indwelling urinary catheter, the risk of CAUTI must be considered and reduced by reviewing the need for the catheter and removing as soon as clinically appropriate (Mantle, 2015). Catheterisation is an aseptic procedure and should only be carried out by a competent healthcare professional trained in urinary catheterisation. Ensuring infection control measures are taken reduces the risk of CAUTI.
Avoiding unnecessary urinary catheterisation prevents the risk of CAUTI. Healthcare professionals should therefore challenge the need for a urinary catheter and ensure that patient assessment is completed before carrying out the procedure. In circumstances where there is a clinical requirement for an indwelling urinary catheter, the risk of CAUTI must be considered and reduced by reviewing the need for the catheter and removing as soon as clinically appropriate (Mantle, 2015). Catheterisation is an aseptic procedure and should only be carried out by a competent healthcare professional trained in urinary catheterisation. Ensuring infection control measures are taken reduces the risk of CAUTI. Providing patients with an indwelling urinary catheter passport can support appropriate catheter care across secondary and primary care settings.
Providing patients with an indwelling urinary catheter passport can support appropriate catheter care across secondary and primary care settings.