References
Bladder and Bowel Community (2017) Toilet Positions. Available online: www.bladderandbowel.org/help-information/resources/toilet-positions
Coloplast (2015) The Cost of Constipation Report. Available online: www.coloplast. co.uk/Global/UK/Continence/Cost_of_ Constipation_Report_FINAL.pdf
Commissioning for incontinence, lower urinary tract and bowel symptoms — an audit (2012). Available online: http://ici-rs.net/PDFs/Commissioningforincontinencel owerurinarytractandbowelsymptomsanaudit_ 2.pdf
Coyne KS, Kaplan SA, Chapple CR, et al (2009) Risk factors and comorbid conditions associated with lower urinary tract symptoms: EpiLUTS. BJU Int 103(3): 24–32
Department of Health (2000) Good practice in continence services. DH, London. Available online: www.nhs.uk/chq/Documents/2015%20uploads/DH%20-%20Good%20practice%20in%20 continence%20services.pdf
Emmanuel A (2004) Constipation. In: Norton C, Chelvanayagam S, eds. Bowel Continence Nursing. Beaconsfield Publishers Ltd. Chap 21: 238–50
European Association of Urology (2011) History examination in neurogenic lower urinary tract dysfunction. Available online: www.uroweb.org/gls/pdf/17_Neurogenic%20LUTS.pdf
Francis R (2010) Robert Francis Inquiry report into Mid-Staffordshire NHS Foundation Trust. Available online: http://webarchive. nationalarchives.gov.uk/20130104234315/ http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_113018
Frattini JC, Nogueras JJ (2008) Slow transit constipation: a review of a colonic functional disorder. Clin Colon Rectal Surg 21(2): 146–52
Harari D (2004) Bowel care in old age. In: Norton C, Chelvanayagam S, eds. Bowel Continence Nursing. Beaconsfield Publishers Ltd. Chap 13: 132–50 Health and Social Care Partnership South East (2011) Prevention and early intervention continence services, July Longstreth G, Thompson G, Chey W, Houghton L, Mearin F and Spiller R (2006) Functional bowel disorder, Gastroenterol 130: 1480–91
NHS Choices (2012) The taboo of incontinence. Available online: www.nhs.uk/Livewell/incontinence/Pages/Breakingthetaboo.aspx
Norton C (2001) Nursing for continence. Beaconsfield Publishers Ltd
Norton C (2006) Constipation in older patients: effects on quality of life. Br J Nurs 15(4): 188–92
Norton C , Chelvanayagam S, eds (2004) Bowel Continence Nursing. Beaconsfield Publishers Ltd, Beaconsfield
Raising Expectations for People with Bladder and Bowel Problems (2015) developed by the Bladder and Bowel Foundation (B&BF), Cystitis and Overactive Bladder Foundation (COB), Association for Continence Advice and expert group on lower urinary tract symptoms (LUTS). London: Astellas Pharma Ltd
Rex J (2013) Treatments for Bowel Dysfunction available on YouTube
Robertson C, Link CL, Onel E, et al (2007) The impact of lower urinary tract symptoms and comorbidities on quality of life: the BACH and UREPIK studies. BJU Int 99(2): 347–54
Royal College of Nursing (2008) Bowel care, including digital rectal examination and manual removal of faeces: RCN guidance for nurses. RCN, London
Royal College of Physicians (2010) National audit of continence care: combined organisational and clinical report. RCP, London. Available online: www.rcplondon.ac.uk/sies/default/files/full-organisational-and-clinical-reportnacc- 2010.pdf



 It is sobering reading, as bladder and bowel dysfunctions lack the same ‘status’ as more recognised chronic conditions, even though the effect of moderate continence issues on quality of life is similar to living with diabetes, hypertension or cancer (Robertson et al, 2007). This means that patients often fail to get even the most basic aspects of care correctly. However, given that poor continence care compromises fundamental NHS rights to dignity and respect, it is essential that addressing these shortcomings must now become a priority. Of the 33 cases presented as oral evidence to the Francis Inquiry into care provided by Mid Staffordshire NHS Foundation Trust, 22 included ‘significant concerns’ about continence care, which led to ‘considerable suffering, distress and embarrassment’ to patients (Francis, 2010).
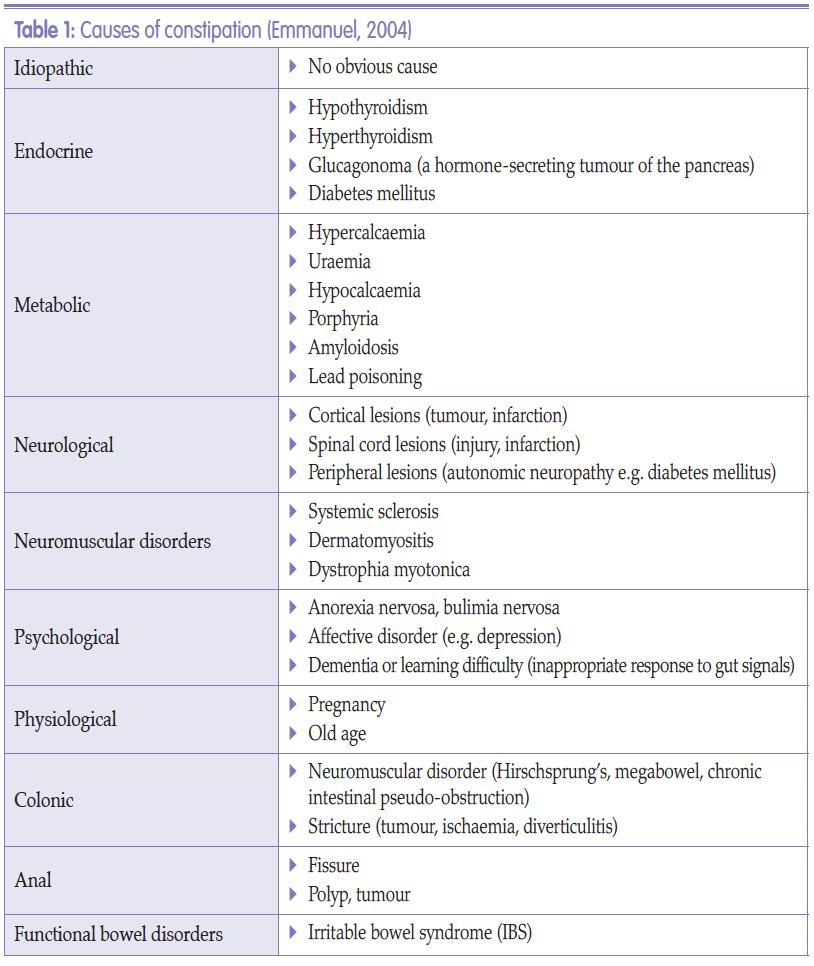
It is sobering reading, as bladder and bowel dysfunctions lack the same ‘status’ as more recognised chronic conditions, even though the effect of moderate continence issues on quality of life is similar to living with diabetes, hypertension or cancer (Robertson et al, 2007). This means that patients often fail to get even the most basic aspects of care correctly. However, given that poor continence care compromises fundamental NHS rights to dignity and respect, it is essential that addressing these shortcomings must now become a priority. Of the 33 cases presented as oral evidence to the Francis Inquiry into care provided by Mid Staffordshire NHS Foundation Trust, 22 included ‘significant concerns’ about continence care, which led to ‘considerable suffering, distress and embarrassment’ to patients (Francis, 2010). Constipation comes in two forms: slow colonic transit or difficulties with evacuation, and it is possible for patients to have both. Those suffering from slow colonic transit tend to complain that they rarely feel the urge to go to the toilet and some cannot go at all unless they take laxatives. According to the Coloplast (2015) report on the cost of constipation, sufferers can be divided into two groups: ‘functional’ and ‘neurogenic’. The majority of people fall into the ‘functional’ category.
Constipation comes in two forms: slow colonic transit or difficulties with evacuation, and it is possible for patients to have both. Those suffering from slow colonic transit tend to complain that they rarely feel the urge to go to the toilet and some cannot go at all unless they take laxatives. According to the Coloplast (2015) report on the cost of constipation, sufferers can be divided into two groups: ‘functional’ and ‘neurogenic’. The majority of people fall into the ‘functional’ category.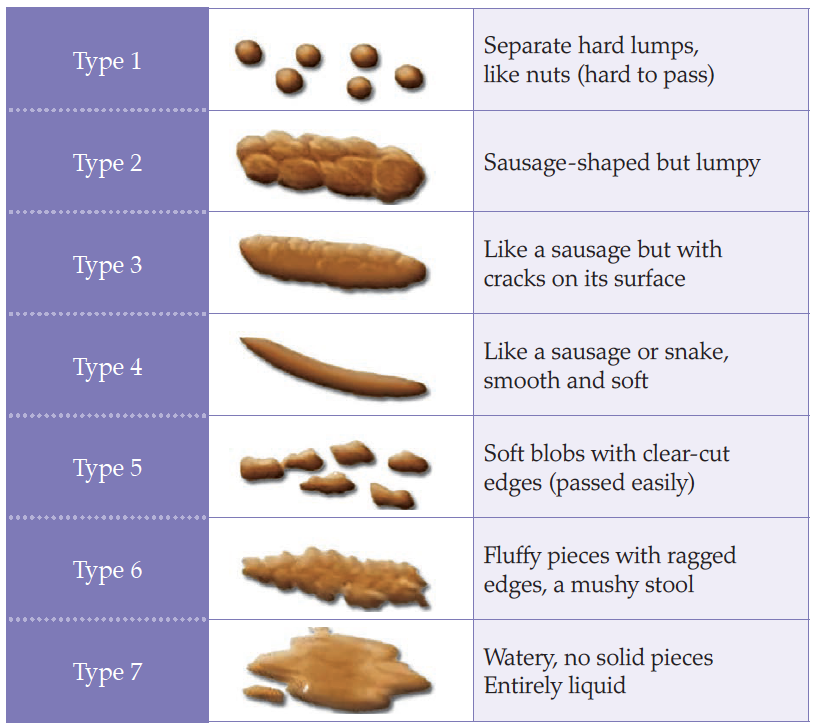
 Obstructive defecation syndrome, or rectal outlet delay, is defined as a sensation of anal blockage on more than one in four occasions, prolonged elimination taking more than 10 minutes to complete evacuation, or the need to use fingers on any occasion (Harari, 2004). Faecal impaction, or loading, is when the rectum and often the lower colon is full of hard or soft stool and the patient is unable to evacuate the bowel unaided (Norton, 2006). This can lead to impaction with overflow ‘spurious diarrhoea’, which is common in the frail elderly population (Harari, 2004) and may be misdiagnosed as diarrhoea and therefore treated incorrectly (Norton, 2006).
Obstructive defecation syndrome, or rectal outlet delay, is defined as a sensation of anal blockage on more than one in four occasions, prolonged elimination taking more than 10 minutes to complete evacuation, or the need to use fingers on any occasion (Harari, 2004). Faecal impaction, or loading, is when the rectum and often the lower colon is full of hard or soft stool and the patient is unable to evacuate the bowel unaided (Norton, 2006). This can lead to impaction with overflow ‘spurious diarrhoea’, which is common in the frail elderly population (Harari, 2004) and may be misdiagnosed as diarrhoea and therefore treated incorrectly (Norton, 2006).