ABSTRACT
Urinary incontinence is prevalent in men, with 61% of the general population of men experiencing lower urinary tract symptoms (LUTS) (NHS England, 2018). These symptoms present as problems with voiding, storage or post-micturition of urine (National Institute for Health and Care Excellence [NICE], 2010). Even after assessment and treatment, some men are still left with urinary incontinence, which is normally managed or contained by either pad products or urinary catheters (if clinically indicated). However, there is a vast range of alternative devices for containment. This article reviews some of the alternative devices that are available, namely sheaths, body worn urinals and penile compression clamps. It discusses the merits and disadvantages of each device and advises when they should or should not be used.KEYWORDS: *Male urinary incontinence *Urinary collecting devices *Male urinary sheath/external catheter, body worn urinals, penile compression devices (clamps)
Most individuals associate the taboo subject of urinary incontinence or bladder leakage with women. This would be due to their numerous risk factors, especially the risks associated with childbirth (Yates, 2017). The condition of urinary incontinence is defined by the International Continence Society (ICS) (Abrams et al, 2002; Haylen et al, 2010) as ‘any involuntary leakage of urine’. However, urinary incontinence is also prevalent in men, with 61% of the general population of men experiencing lower urinary tract symptoms (LUTS) (NHS England, 2018). Lower urinary tract symptoms present as problems with voiding, storage or post-micturition of urine (NICE, 2010). Voiding symptoms include weak or intermittent urinary stream, straining, hesitancy, terminal dribbling and incomplete emptying. Storage symptoms include urgency, frequency, urge incontinence and nocturia/nocturnal enuresis (either waking to void at night or loss of urine during sleep). The major post-micturition symptom is postmicturition dribbling (an involuntary loss of urine immediately after the person has finished passing urine), which is common and bothersome (NICE, 2010).
There are many possible causes of LUTS, such as abnormalities or dysfunction of the prostate (including enlarged prostate or cancer of prostate), urethra, bladder or sphincters. Other conditions which include detrusor muscle weakness (or overactivity), urinary tract infections (UTIs), prostate inflammation (prostatitis) and neurological disease (e.g. cerebrovascular accident, spinal injury, multiple sclerosis, dementia) (NICE, 2010) can also affect the function of the lower urinary tract.
There are many possible causes of LUTS, such as abnormalities or dysfunction of the prostate (including enlarged prostate or cancer of prostate), urethra, bladder or sphincters. Other conditions which include detrusor muscle weakness (or overactivity), urinary tract infections (UTIs), prostate inflammation (prostatitis) and neurological disease (e.g. cerebrovascular accident, spinal injury, multiple sclerosis, dementia) (NICE, 2010) can also affect the function of the lower urinary tract.
Men may be reluctant to seek help with this problem, which is extremely distressing. It can have a negative impact on quality of life, including devastating physical effects, such as association with long-term morbidities, UTIs, falls and increased hospital stays (Macaulay et al, 2015). Urinary incontinence can also have psychological, social and financial implications for both the individual and their family (Lukacz et al, 2011; Yates, 2019). For men who cannot regain continence after treatment, collecting devices or equipment, which usually means pads or catheters, are advised to maintain social continence (Macaulay et al, 2015).
However, in the author’s clinical experience, there is a whole range of other devices/equipment available that may be far more acceptable and suitable to the individual’s personal needs. Healthcare professionals are in an ideal position to offer advice on correct devices/equipment, but only if they have the relevant knowledge regarding different types of devices/ equipment available and how to use correctly. This article discusses some of these devices, namely sheaths, body worn urinals and penile clamps.
However, in the author’s clinical experience, there is a whole range of other devices/equipment available that may be far more acceptable and suitable to the individual’s personal needs. Healthcare professionals are in an ideal position to offer advice on correct devices/equipment, but only if they have the relevant knowledge regarding different types of devices/ equipment available and how to use correctly. This article discusses some of these devices, namely sheaths, body worn urinals and penile clamps.
ASSESSMENT
Before being advised about any form of management device or collecting equipment, an individual continence assessment should be undertaken both to rule out any red flag presenting symptoms, and to assess the amount of incontinence to provide a device/product suitable for the individual. The initial assessment, as recommended by NICE (2010), should include the individual’s previous medical/surgical history, taking into account any comorbidities, medication taken, including over-the-counter or herbal, bladder diary/frequency volume chart, urinalysis to detect any glucose, protein, blood etc, and physical examination of abdomen, external genitalia and digital rectal examination (DRE) of the prostate. Advice should also be given about prostate specific antigen testing (PSA). Red flag symptoms should be identified early during assessment. These include (but are not exclusive) and may be used in conjunction with other investigations, i.e. prostate examination, blood results:- Haematuria (blood in the urine)
- Blood in the semen
- Painful burning sensation on urination/ejaculation
- Increased frequency especially at night
- Increased urgency
- Difficulty to start flow or straining to pass urine, hesitancy or weak flow.
MANAGEMENT
While treatment options are always the best outcome, not all urinary incontinence can be cured completely and even those who are successfully treated may have to endure incontinence for a time (ICS, 2017). The continence issue should then be appropriately managed by either collecting devices/equipment, pad products, or urinary catheters. This article does not have enough scope to look at pad products or urinary catheters, so will only discuss devices/equipment.Due to the many different types of devices available, the choice for healthcare professionals to select an appropriate one can be confusing and overwhelming. Thus, information from resources such as specialist continence nurses, literature or via individual companies’ learning packages can be helpful. These devices and products will now be discussed individually, but for further information, the ICS has collaborated to make information available via a web site hosted by the ICS at: www.continenceproductadvisor.org.
Urinary sheaths
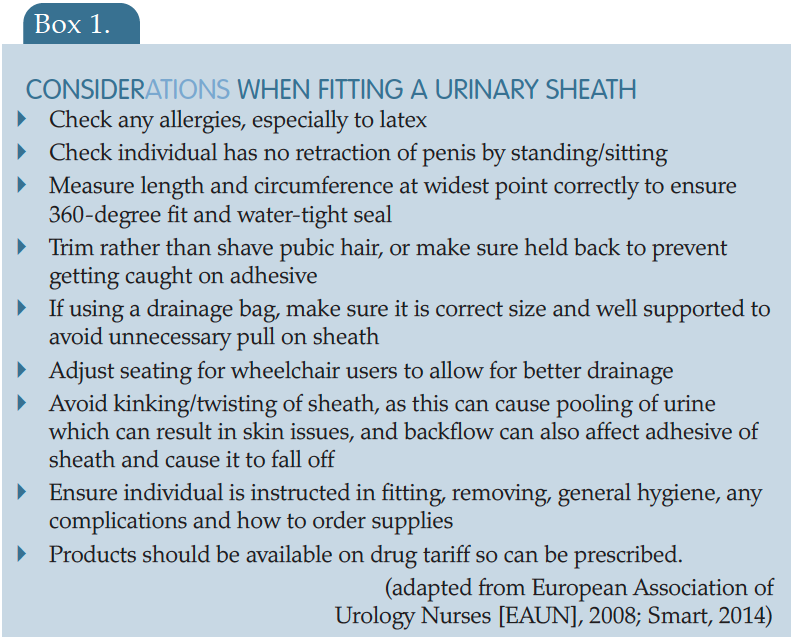
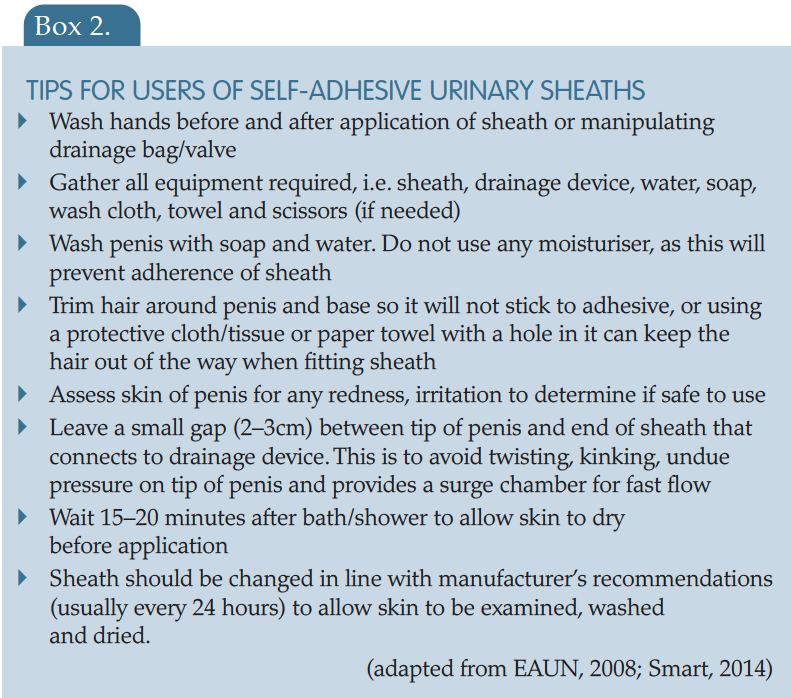
Sheaths, also known as male external catheters (MEC), look in appearance similar to a contraceptive condom (Figure 1). These devices are soft, flexible sleeves designed to fit over the penis and can be attached to a urinary drainage bag or valve. It is vitally important that healthcare professionals are competent in assessing the need for a sheath and have the skill and expertise in applying correctly and passing this knowledge onto the individual. Urinary sheaths have specialised features that need to be considered before being recommended to an individual for use (Table 1).
Figure 1.
Urinary sheaths
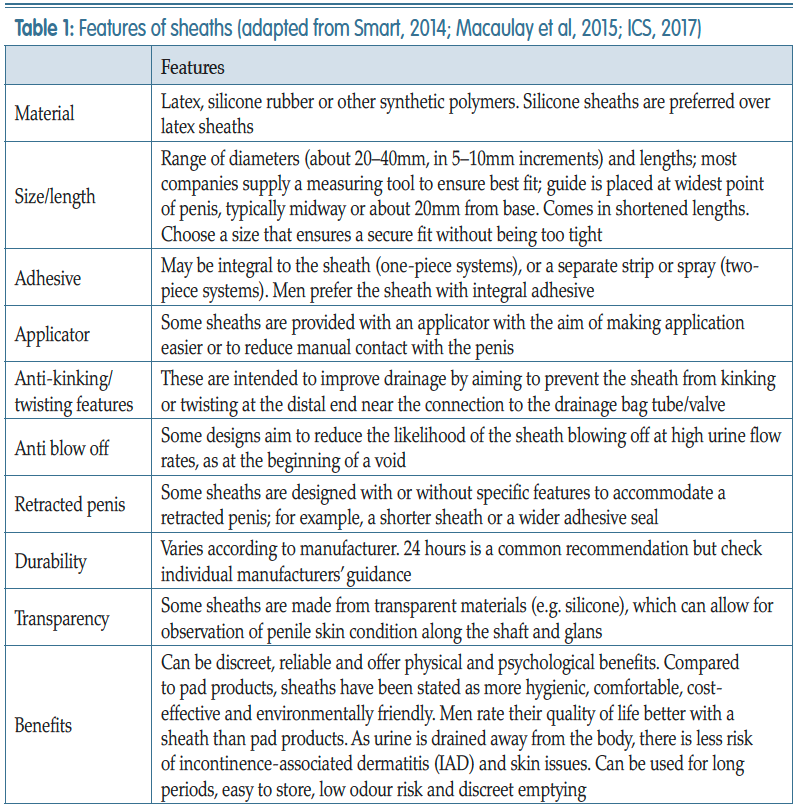
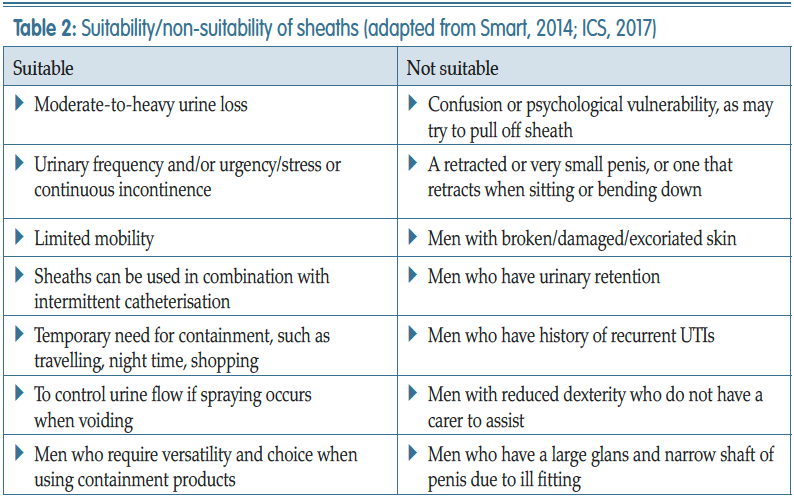
To use a sheath, individuals should have good dexterity, some degree of penile length (no retraction), usually have moderate-to-severe urinary incontinence, suffer with urinary urgency/frequency, and find it difficult to get to the toilet in time. Men may use for temporary containment, i.e. travel, shopping or during the night. However there are also some men for whom sheaths would not be advisable or suitable (Table 2).
While numerous benefits have been identified for using a sheath system (Smart, 2014; Macaulay et al, 2015), there are also some disadvantages, including:
- Contact dermatitis, which can arise from allergy developing over time especially to latex
- Compression or tourniquet effect due to ill-fitting sheath or use with individuals with little or no penile sensation
- Difficult to apply/painful to remove (Macaulay et al, 2015)
- Skin irritation due to sheath twisting and stagnation of urine causing urine to be in contact with penile skin
- Pressure ulcers on glans due to ill- fitting sheath
- Sexual activity may be limited (Smart, 2014).
Body worn urinals (BWU)
When a sheath system is considered unsuitable due to penile retraction, which is common in older men or those who have had treatment for prostate cancer, there are alternatives. These come in the form of modified sheaths, pubic pressure urinals, or penile pouches. The devices are useful for men who are unable to wear a sheath and do not wish to wear pad products or wish to leave the house and toilet access may be an issue.The modified sheath (petal sheath, Figure 2) follows the fitting guide of the sheath (Box 2) with regards to skin preparation and can be used on individuals with penile retraction.
Pubic pressure urinals (PPU)
These are made from latex and are washable/reusable. They consist of a pressure ring (or doughnut), which is held in place by straps or underwear. The ring applies pressure to the pubic area and helps the penis to protrude into the cone device (Figure 3).These are suitable for men who have:
- A retracted penis, for whom a sheath would not be suitable
- Moderate-to-heavy urine loss
- Urinary frequency and/or urgency
- A preference to use a body worn urinal rather than absorbent products during the day
- The ability to walk but may have the ability to sit out in a chair during the daytime.
These devices usually require specialised fittings for patients by trained staff and there are particular challenges. These include maintaining a secure fit, preventing the penis slipping out of the device, kinking and twisting of the tubing attached to the cone, as well as the risk of skin damage (ICS, 2017).

Figure 2
Petal sheaths

Figure 3
PPU with drainage bag.
For the device to be effective, the ICS (2017) recommend that the user/ carer should:
- Understand how to use the device and the importance of skin care
- Have good manual dexterity to manage the device
- Have fitting done by a specialist to ensure best leak-proof fit
- Have moderate-to-heavy urine loss
- Have urinary frequency and/ or urgency
- Have limited mobility.
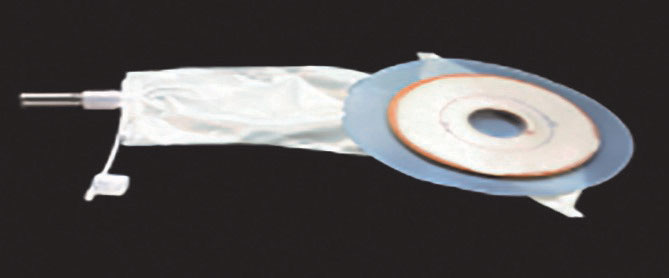
Figure 4
Penile pouch
.jpg)
Figure 5
Range of penile compression clamps
Penile pouches
These are small disposable collection bags, with an adhesive ring that is stuck over the penis and attached to the pubic bone (Figure 4).It is necessary to shave the pubic area for the adhesive to make a good seal. The hole fitting over the penis can be cut to size. The pouch collects urine, which can be emptied via the small tap into the toilet, or the tap can be connected to a larger urine drainage bag if required. They can usually stay in place for 24–48 hours, but manufacturers’ guidance should be adhered to.
Penile compression clamps
These are often referred to as male mechanical devices or penile clamps, and are the only device discussed here which may not be available on prescription. They are small reusable devices in different designs and are available via different manufacturers. They are designed to prevent urine leakage by compressing the penile urethra (Figure 5).They should be fitted to the middle or base of the penis. While many are adjustable, others are available in different sizes. It may take some trial and error to get the correct fitting device. Penile clamps are more likely to suit men who do not want to wear a sheath or pad product, have sufficient length of penis to attach device, wish to prevent leakage for a specific period, i.e. exercise, swimming etc, and who suffer with mainly stress urinary incontinence and feel that preventing leakage is more important than containment (Continence product advisor, 2020). However, these devices are less likely to suit individuals if their leakage is associated with urgency, they have poor memory or mental function, poor dexterity, skin prone to damage and no bladder sensation to void (Continence product advisor, 2020).
These devices should be used with caution, due to reduced penile blood flow and potential pressure injury damage to the skin (Lemmens et al, 2019). Lemmens et al (2019) recommend a period of 60 minutes wearing the device, and then the same recovery time without the device applied. They are not recommended for overnight use.
Careful assessment is necessary for use of these devices, and they should be fitted by a trained healthcare professional and re-evaluated on a regular basis. However, in the author’s clinical experience, there are few healthcare professional who are aware of these devices, so advice via the manufacturer may be required. These devices are usually more beneficial when used in conjunction with other containment devices, e.g. pad products.
Careful assessment is necessary for use of these devices, and they should be fitted by a trained healthcare professional and re-evaluated on a regular basis. However, in the author’s clinical experience, there are few healthcare professional who are aware of these devices, so advice via the manufacturer may be required. These devices are usually more beneficial when used in conjunction with other containment devices, e.g. pad products.
CONCLUSION
There are numerous devices, other than indwelling catheters or pads, which may be suitable for men to contain their urinary incontinence. As a healthcare professional, it is important to know which devices are available, and how to use them, to be able to advise individual patients about what may be suitable for them to improve their quality of life. This article has looked at some of the devices available and the importance of individual assessment to recommend the correct device.KEY POINTS
- Urinary incontinence in men is common and increases with age
- Men are reluctant to discuss this problem and engage with professionals, so sensitivity, tact and knowledge of the condition is essential when assessing
- Healthcare professionals should be aware of the different types of urinary containment devices
- Healthcare professionals should understand the benefits and disadvantages of the different devices for managing urinary incontinence
- An individual’s quality of life can be greatly improved by a knowledgeable healthcare professional providing the correct advice and support.
This piece was first published in the Journal of Community Nursing. To cite this article use: Yates Y (2020) Managing male urinary incontinence with sheaths, body worn urinals and penile compression clamps. J Community Nurs 34(5): 52-58
References
Abrams P, Cardozo L, Fall M, et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Subcommittee of the International Continence Society. Neurourol Urodyn 21(2): 167–178
Continence Product Advisor (2020) Penile compression devices. Available online: www.continenceproductadvisor.org/products/maledevices/penilecompressiondevices
European Association of Urology Nurses (2008) Good Practice in Health Care: The male external catheter. Available online: https://nurses.uroweb.org/wp-content/uploads/EAUN_MEC_Guidelines_EN_2008_LR.pdf
Haylen BT, de Ridder D, Freeman RM, et al (2010) An international urogynecological association (IUGA)/ international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29(1): 4–20
International Continence Society (2017) Incontinence. 6th edn. Editors Abrams P, Cardozo L, Wagg A, Wein A, ICUD ICS Tokyo
Lemmens JMH, Broadbridge J, Macaulay M, Rees RW, Archer M, Drake MJ, Moore KN, Bader DL, Fader M (2019) Tissue response to applied loading using different designs of penile compression clamps. Med Devices (Auckl) 12: 235–243
Lukacz ES, Sampselle C, Gray M, et al (2011) A healthy bladder: a consensus statement. Int J Clin Prac 65(10): 1026–1036
Macaulay M, Broadbridge J, Gage H, Williams P, Birch B, Moore KN, Cottenden A, Fader M (2015) A trial of devices for urinary incontinence after treatment for prostate cancer. BJU Int 116: 432–442
NHS England (2018) Excellence in continence care: Practical guidance for commissioners, and leaders in health and social care. Available online: www.england.nhs.uk/wp-content/uploads/2018/07/excellence-in-continence-care.pdf
National Institute for Health and Care Excellence (2010) Lower urinary tract symptoms in men: management. Clinical Guideline CG97 updated in 2015. Available online: https://www.nice.org.uk/Guidance/CG97
Smart C (2014) Male urinary incontinence and the urinary sheath. Br J Nurs Urol Supp 23(9): S20–S25
Yates A (2017) Urinary continence care for the older people in the acute setting. Br J Nurs 26(9 suppl): S28–S30
Yates A (2019) Basic continence assessment: what community nurses should know. J Community Nurs 33(3): 52–55
Continence Product Advisor (2020) Penile compression devices. Available online: www.continenceproductadvisor.org/products/maledevices/penilecompressiondevices
European Association of Urology Nurses (2008) Good Practice in Health Care: The male external catheter. Available online: https://nurses.uroweb.org/wp-content/uploads/EAUN_MEC_Guidelines_EN_2008_LR.pdf
Haylen BT, de Ridder D, Freeman RM, et al (2010) An international urogynecological association (IUGA)/ international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29(1): 4–20
International Continence Society (2017) Incontinence. 6th edn. Editors Abrams P, Cardozo L, Wagg A, Wein A, ICUD ICS Tokyo
Lemmens JMH, Broadbridge J, Macaulay M, Rees RW, Archer M, Drake MJ, Moore KN, Bader DL, Fader M (2019) Tissue response to applied loading using different designs of penile compression clamps. Med Devices (Auckl) 12: 235–243
Lukacz ES, Sampselle C, Gray M, et al (2011) A healthy bladder: a consensus statement. Int J Clin Prac 65(10): 1026–1036
Macaulay M, Broadbridge J, Gage H, Williams P, Birch B, Moore KN, Cottenden A, Fader M (2015) A trial of devices for urinary incontinence after treatment for prostate cancer. BJU Int 116: 432–442
NHS England (2018) Excellence in continence care: Practical guidance for commissioners, and leaders in health and social care. Available online: www.england.nhs.uk/wp-content/uploads/2018/07/excellence-in-continence-care.pdf
National Institute for Health and Care Excellence (2010) Lower urinary tract symptoms in men: management. Clinical Guideline CG97 updated in 2015. Available online: https://www.nice.org.uk/Guidance/CG97
Smart C (2014) Male urinary incontinence and the urinary sheath. Br J Nurs Urol Supp 23(9): S20–S25
Yates A (2017) Urinary continence care for the older people in the acute setting. Br J Nurs 26(9 suppl): S28–S30
Yates A (2019) Basic continence assessment: what community nurses should know. J Community Nurs 33(3): 52–55


