References
All Party Parliamentary Group for Continence Care Report (2011) Cost-effective Commissioning for Continence Care. Available online: http://176.32.230.26/appgcontinence.org.uk/wp-content/uploads/2020/02/CommissioningGuideWEB.pdf
Department of Health (DH) (2000) Good practice in continence services. Available online: https://www.nhs.uk/chq/documents/2015%20uploads/dh%20-%20good%20practice%20in%20continence%20services.pdf
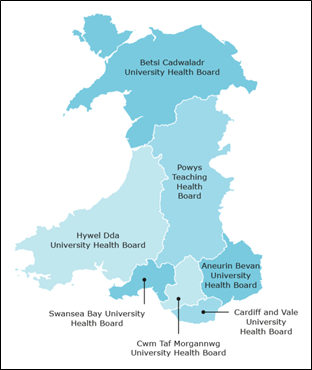
Doheny S (2015) The organisation of the NHS in the UK: comparing structures in the four countries. National Assembly for Wales. Available online: https://senedd.wales/research%20documents/15-020%20-%20the%20organisation%20of%20the%20nhs%20in%20the%20uk%20comparing%20structures%20in%20the%20four%20countries/15-020.pdf
NHS England (2021) Integrated Care Systems: design framework. Available online: https://www.england.nhs.uk/wp-content/uploads/2021/06/B0642-ics-design-framework-june-2021.pdf
NHS Wales (2006) All Wales Bladder and Bowel Care Pathway
NHS Wales (2016) Patient urinary catheter passport: looking after your urinary catheter. Available online: https://phw.nhs.wales/services-and-teams/harp/urinary-tract-infection-uti-resources-and-tools/uti-downloads/patient-catheter-passport-for-wales-english-version/
NHS Wales (2020) NHS Wales Annual Planning Framework 2021 – 2022. Available online: https://gov.wales/sites/default/files/publications/2021-01/nhs-wales-annual-planning-framework-2021-2022.pdf
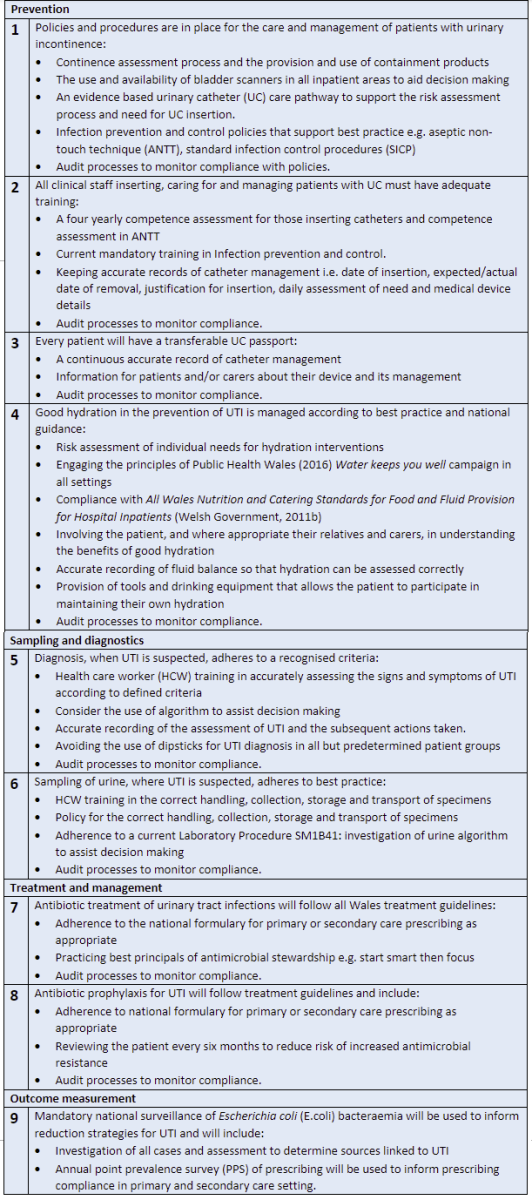
Public Health Wales (2018) UTI 9 Key Standards for UTI Prevention, Treatment and Management. Available online: https://phw.nhs.wales/services-and-teams/harp/urinary-tract-infection-uti-resources-and-tools/uti-downloads/uti-9-key-standards-for-uti-prevention-treatment-and-management1/
Public Health Wales (2016) Water keeps you well. Available online: http://www.wales.nhs.uk/news/40453
Public Health England (2021) Exploring the implementation of interventions to reduce catheter-associated urinary tract infections (ENACT). Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1017534/ENACT_CAUTI_report.pdf
Shapiro J. (2010) The NHS: the story so far (1948 – 2010). Clin Med 10(4): 336 – 338
Welsh Government (2002) The Report from the Advisory Group on a Strategy for Older People in Wales, When I’m 64......and more. Available online: https://www.iwa.wales/agenda/2010/10/when-im-sixty-four/
Welsh Government (2011a) The indignity of incontinence: local information pack for assembly members. Available online: https://business.senedd.wales/documents/s43157/Consultation%20response%20RC%2016%20-%20All%20Wales%20Continence%20Forum%20AWCF.pdf
Welsh Government (2011b) All Wales Nutrition and Catering Standards for Food and Fluid Provision for Hospital Inpatients. Available online: http://www.wales.nhs.uk/sitesplus/documents/862/FOI-077e-15.pdf
Department of Health (DH) (2000) Good practice in continence services. Available online: https://www.nhs.uk/chq/documents/2015%20uploads/dh%20-%20good%20practice%20in%20continence%20services.pdf
Doheny S (2015) The organisation of the NHS in the UK: comparing structures in the four countries. National Assembly for Wales. Available online: https://senedd.wales/research%20documents/15-020%20-%20the%20organisation%20of%20the%20nhs%20in%20the%20uk%20comparing%20structures%20in%20the%20four%20countries/15-020.pdf
NHS England (2021) Integrated Care Systems: design framework. Available online: https://www.england.nhs.uk/wp-content/uploads/2021/06/B0642-ics-design-framework-june-2021.pdf
NHS Wales (2006) All Wales Bladder and Bowel Care Pathway
NHS Wales (2016) Patient urinary catheter passport: looking after your urinary catheter. Available online: https://phw.nhs.wales/services-and-teams/harp/urinary-tract-infection-uti-resources-and-tools/uti-downloads/patient-catheter-passport-for-wales-english-version/
NHS Wales (2020) NHS Wales Annual Planning Framework 2021 – 2022. Available online: https://gov.wales/sites/default/files/publications/2021-01/nhs-wales-annual-planning-framework-2021-2022.pdf
Public Health Wales (2018) UTI 9 Key Standards for UTI Prevention, Treatment and Management. Available online: https://phw.nhs.wales/services-and-teams/harp/urinary-tract-infection-uti-resources-and-tools/uti-downloads/uti-9-key-standards-for-uti-prevention-treatment-and-management1/
Public Health Wales (2016) Water keeps you well. Available online: http://www.wales.nhs.uk/news/40453
Public Health England (2021) Exploring the implementation of interventions to reduce catheter-associated urinary tract infections (ENACT). Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1017534/ENACT_CAUTI_report.pdf
Shapiro J. (2010) The NHS: the story so far (1948 – 2010). Clin Med 10(4): 336 – 338
Welsh Government (2002) The Report from the Advisory Group on a Strategy for Older People in Wales, When I’m 64......and more. Available online: https://www.iwa.wales/agenda/2010/10/when-im-sixty-four/
Welsh Government (2011a) The indignity of incontinence: local information pack for assembly members. Available online: https://business.senedd.wales/documents/s43157/Consultation%20response%20RC%2016%20-%20All%20Wales%20Continence%20Forum%20AWCF.pdf
Welsh Government (2011b) All Wales Nutrition and Catering Standards for Food and Fluid Provision for Hospital Inpatients. Available online: http://www.wales.nhs.uk/sitesplus/documents/862/FOI-077e-15.pdf