References
Beeckman D, Campbell J, Campbell K, et al (2015) Proceedings of the Global IAD Expert Panel. Incontinence Associated Dermatitis: Moving Prevention Forward. Wounds International, London
Beeckman D, Van den Bussche K, Alves P, et al (2018) Towards an international language for incontinence-associated dermatitis (IAD): design and evaluation of psychometric properties of the Ghent Global IAD Categorization Tool (GLOBIAD) in 30 countries. Br J Dermatol 178(6): 1331–40
Cutting K, Westgate SJ (2012) The use of wound cleansing solutions in chronic wounds. Wounds UK 8: 130–3
Dhoonmoon L, Dyer M (2020) Improving leg ulcer care in the community. J Community Nurs 34(6): 40–4
Fletcher J, Beeckman D, Boyles A (2020) International Best Practice Recommendations. Prevention and management of moistureassociated skin damage (MASD). Wounds International. Available online: www.woundsinternationalcom
Francis K (2019) Damage control: Differentiating incontinence-associated dermatitis from pressure injury. Nursing 14(6): 18–25
Glass GF Jr, Goh CCK, Cheong RQ, Ong ZL, Khong PCB, Chan EY (2021) Effectiveness of skin cleanser and protectant regimen on incontinenceassociated dermatitis outcomes in acute care patients: A cluster randomised trial. Int Wound J 18(6): 862–73 (published correction appears in Int Wound J [2022] 19(7): 1955)
Gov.UK (2021) Ethnicity facts and figures. Available online: www.ethnicity-factsfigures.service.gov.uk/
Gray M, Black JM, Baharestani MM, et al (2011) Moisture-associated skin damage: overview and pathophysiology. J Wound Ostomy Continence Nurs 38(3): 233–41
Green M, Kashetsky N, Feschuk A, Maibach HI (2022) Transepidermal water loss (TEWL): environment and pollution - A systematic review. Skin Health Dis 2(2): e104
Gupta V, Sharma VK (2019) Skin typing: Fitzpatrick grading and others. Clin Dermatol 37(5): 430–6
Ho BK, Robinson JK (2015) Color bar tool for skin type self-identification: A crosssectional study. J Am Acad Dermatol 73(2): 312–3
Lopez-Ojeda W, Pandey A, Alhajj M, et al (2022) Anatomy, Skin (Integument) [Updated 2022 Oct 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available online: www.ncbi.nlm.nih.gov/books/NBK441980/
Meyer I, Richter HE (2015) Impact of fecal incontinence and its treatment on quality of life in women. Womens Health (Lond) 11(2): 225–38
Moore Z, Bell T, Carville K, et al (2015) International Best Practice Statement: Optimising patient involvement in wound management. Wounds International, London
Mukwende M (2020) Mind the Gap: a clinical handbook of signs and symptoms in black and brown skin. Wounds UK 16(3): 16
Nakagami G, Sanada H, Kitagawa A, et al (2006) Incontinence induces stratum corneum vulnerability and impairs the skin barrier function in the perianal region. Dermatology 213(4): 293–9
NHS England (2018) Excellence in Continence Care. Available online: www.england.nhs.uk/wp-content/uploads/2018/07/excellence-in-continence-care.pdf
Nijhawan R, Alexis A (2011) Practical approaches to medical and cosmetic dermatology in skin of color patients. Expert Rev Dermatol 6: 175–87
Norton C, Thomas L, Hill J (2007) Guideline Development Group. Management of faecal incontinence in adults: summary of NICE guidance. BMJ 334(7608): 1370–71
Vanscheidt W, Harding K, Teot L, Siebert J (2012) Effectiveness and tissue compatibility of a 12-week treatment of chronic venous leg ulcers with an octenidine based antiseptic — a randomized, double-blind controlled study. Int Wound J 9(3): 316–23
Waller S, Cole N (2023) Versatility of a skin protectant ointment in managing moisture-associated skin damage caused by incontinence. Wounds UK 19(1): 58–63
Woo KY, Beeckman D, Chakravarthy D (2017) Management of moistureassociated skin damage: a scoping review. Adv Skin Wound care 30(11): 494–501
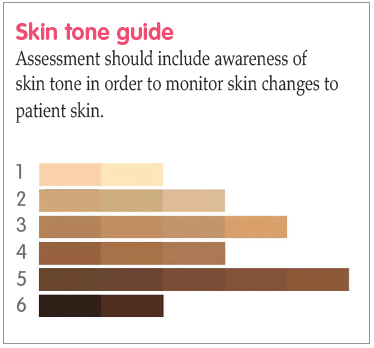
Wounds UK (2021) Best Practice Statement: Addressing skin tone bias in wound care: assessing signs and symptoms in people with dark skin tones. Wounds UK, London. Available online: www.wounds-uk.com
Woodward S, Norton C (2020) New study into treatment and prevention of incontinence-associated dermatitis. King’s College, London. Available online: www.kcl.ac.uk/news/new-studyinto-treatment-and-prevention-ofincontinence-associated-dermatitis
Young T (2017) Back to basics: understanding moisture-associated skin damage. Wounds UK 13(2): 56–65
Beeckman D, Van den Bussche K, Alves P, et al (2018) Towards an international language for incontinence-associated dermatitis (IAD): design and evaluation of psychometric properties of the Ghent Global IAD Categorization Tool (GLOBIAD) in 30 countries. Br J Dermatol 178(6): 1331–40
Cutting K, Westgate SJ (2012) The use of wound cleansing solutions in chronic wounds. Wounds UK 8: 130–3
Dhoonmoon L, Dyer M (2020) Improving leg ulcer care in the community. J Community Nurs 34(6): 40–4
Fletcher J, Beeckman D, Boyles A (2020) International Best Practice Recommendations. Prevention and management of moistureassociated skin damage (MASD). Wounds International. Available online: www.woundsinternationalcom
Francis K (2019) Damage control: Differentiating incontinence-associated dermatitis from pressure injury. Nursing 14(6): 18–25
Glass GF Jr, Goh CCK, Cheong RQ, Ong ZL, Khong PCB, Chan EY (2021) Effectiveness of skin cleanser and protectant regimen on incontinenceassociated dermatitis outcomes in acute care patients: A cluster randomised trial. Int Wound J 18(6): 862–73 (published correction appears in Int Wound J [2022] 19(7): 1955)
Gov.UK (2021) Ethnicity facts and figures. Available online: www.ethnicity-factsfigures.service.gov.uk/
Gray M, Black JM, Baharestani MM, et al (2011) Moisture-associated skin damage: overview and pathophysiology. J Wound Ostomy Continence Nurs 38(3): 233–41
Green M, Kashetsky N, Feschuk A, Maibach HI (2022) Transepidermal water loss (TEWL): environment and pollution - A systematic review. Skin Health Dis 2(2): e104
Gupta V, Sharma VK (2019) Skin typing: Fitzpatrick grading and others. Clin Dermatol 37(5): 430–6
Ho BK, Robinson JK (2015) Color bar tool for skin type self-identification: A crosssectional study. J Am Acad Dermatol 73(2): 312–3
Lopez-Ojeda W, Pandey A, Alhajj M, et al (2022) Anatomy, Skin (Integument) [Updated 2022 Oct 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available online: www.ncbi.nlm.nih.gov/books/NBK441980/
Meyer I, Richter HE (2015) Impact of fecal incontinence and its treatment on quality of life in women. Womens Health (Lond) 11(2): 225–38
Moore Z, Bell T, Carville K, et al (2015) International Best Practice Statement: Optimising patient involvement in wound management. Wounds International, London
Mukwende M (2020) Mind the Gap: a clinical handbook of signs and symptoms in black and brown skin. Wounds UK 16(3): 16
Nakagami G, Sanada H, Kitagawa A, et al (2006) Incontinence induces stratum corneum vulnerability and impairs the skin barrier function in the perianal region. Dermatology 213(4): 293–9
NHS England (2018) Excellence in Continence Care. Available online: www.england.nhs.uk/wp-content/uploads/2018/07/excellence-in-continence-care.pdf
Nijhawan R, Alexis A (2011) Practical approaches to medical and cosmetic dermatology in skin of color patients. Expert Rev Dermatol 6: 175–87
Norton C, Thomas L, Hill J (2007) Guideline Development Group. Management of faecal incontinence in adults: summary of NICE guidance. BMJ 334(7608): 1370–71
Vanscheidt W, Harding K, Teot L, Siebert J (2012) Effectiveness and tissue compatibility of a 12-week treatment of chronic venous leg ulcers with an octenidine based antiseptic — a randomized, double-blind controlled study. Int Wound J 9(3): 316–23
Waller S, Cole N (2023) Versatility of a skin protectant ointment in managing moisture-associated skin damage caused by incontinence. Wounds UK 19(1): 58–63
Woo KY, Beeckman D, Chakravarthy D (2017) Management of moistureassociated skin damage: a scoping review. Adv Skin Wound care 30(11): 494–501
Wounds UK (2021) Best Practice Statement: Addressing skin tone bias in wound care: assessing signs and symptoms in people with dark skin tones. Wounds UK, London. Available online: www.wounds-uk.com
Woodward S, Norton C (2020) New study into treatment and prevention of incontinence-associated dermatitis. King’s College, London. Available online: www.kcl.ac.uk/news/new-studyinto-treatment-and-prevention-ofincontinence-associated-dermatitis
Young T (2017) Back to basics: understanding moisture-associated skin damage. Wounds UK 13(2): 56–65