Continence is an individual’s voluntary control of their bladder or bowel. It is a crucial part of dignity and a firmly entrenched societal norm. We are born without it and develop it as we mature into early childhood; intense embarrassment can exist for those who lose or never gain this control, making it hard for them to reach out to health and social care workers who can help them adapt to, resolve, or manage this problem.
With a focus on urinary incontinence in adults, this article explores recent best practice guidance to help healthcare professionals, who have contact with people with continence needs, to be aware of their role and responsibilities and the best practice standards available to guide training and development in the delivery of continence assessment and management.
The United Kingdom Continence Society (UKCS) 2015 minimum standards document states that those with continence care needs should be assessed with the goal of making a diagnosis and offering treatment, and that it is only in a minority of cases that this goal of treating and resolving the problem may need modifying to a goal of managing the symptoms. It is tragic, therefore, that many people with continence needs still suffer in silence. The British Association of Urological Surgeons (BAUS) estimates that around three million people in the UK experience urinary incontinence and, of these, as many as 60–80% have never sought medical advice for their condition. Often, they just see it as part of the aging process (BAUS, 2018).
The ‘Five Year Forward View’ document encourages health and social care to work in tandem, utilising the many resources the third sector has to offer and empowering people to have greater input and choice around the management of their condition (NHS England, 2014). This model is ideal for continence care and should guide healthcare professionals’ approach to achieving an excellent service for people.
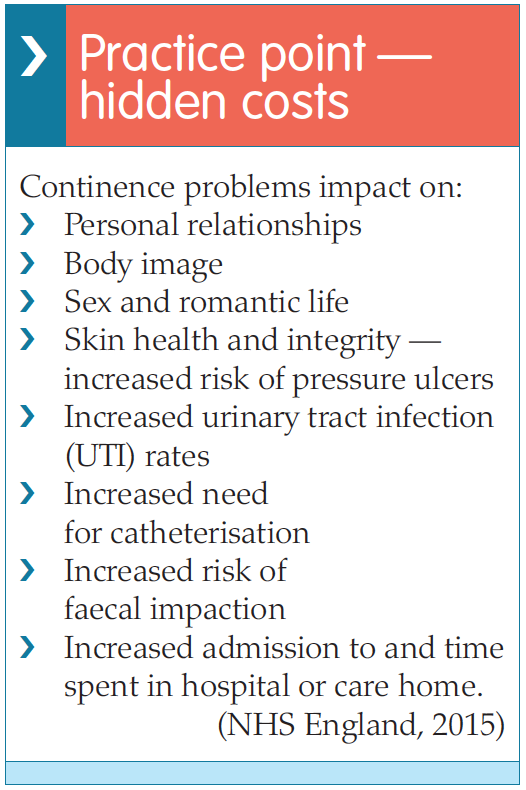
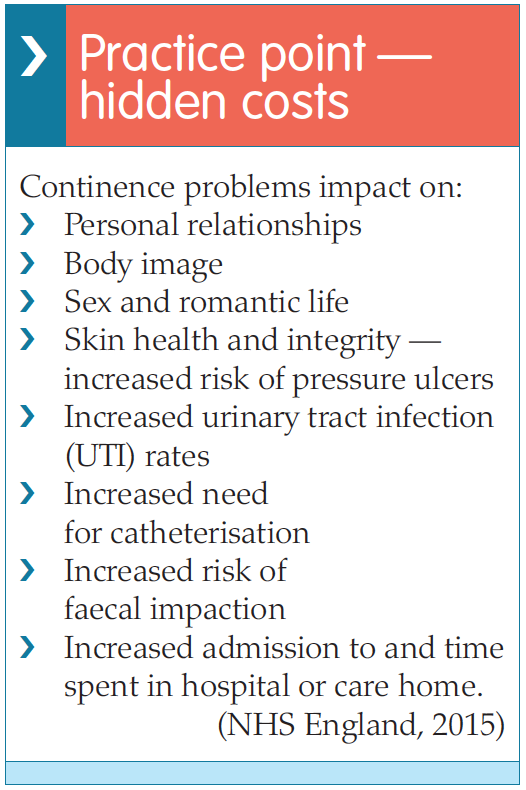
There are many advantages in providing excellent continence care. In their guidance document,NHS England (2015) conclude that improved continence care with integrated services across primary, secondary and care home settings will produce the following benefits:
With a focus on urinary incontinence in adults, this article explores recent best practice guidance to help healthcare professionals, who have contact with people with continence needs, to be aware of their role and responsibilities and the best practice standards available to guide training and development in the delivery of continence assessment and management.
The United Kingdom Continence Society (UKCS) 2015 minimum standards document states that those with continence care needs should be assessed with the goal of making a diagnosis and offering treatment, and that it is only in a minority of cases that this goal of treating and resolving the problem may need modifying to a goal of managing the symptoms. It is tragic, therefore, that many people with continence needs still suffer in silence. The British Association of Urological Surgeons (BAUS) estimates that around three million people in the UK experience urinary incontinence and, of these, as many as 60–80% have never sought medical advice for their condition. Often, they just see it as part of the aging process (BAUS, 2018).
The ‘Five Year Forward View’ document encourages health and social care to work in tandem, utilising the many resources the third sector has to offer and empowering people to have greater input and choice around the management of their condition (NHS England, 2014). This model is ideal for continence care and should guide healthcare professionals’ approach to achieving an excellent service for people.
There are many advantages in providing excellent continence care. In their guidance document,NHS England (2015) conclude that improved continence care with integrated services across primary, secondary and care home settings will produce the following benefits:
- A better quality of life and more independence through finding solutions appropriate to individual needs
- Less reliance on pads and products by using alternative treatments
- A reduction in admission to hospital and care homes
- Fewer complications, such as urinary tract infections (UTIs), faecal impaction and skin breakdown
- A reduction in costs (NHS England, ‘Excellence in continence care’ [EICC], 2015).
WHAT SHOULD BE DONE IN THE COMMUNITY?
Case finding
Embarrassment and a lack of awareness of the possibility of improving or even curing continence problems often blocks an individual’s ability to seek help for their condition. Being aware of who is at risk and asking the right questions is therefore an important part of clinical assessment (NHS England, 2015).It is vital to screen for continence issues in the following populations (NHS England, 2015):
- Children and young people
- Pregnant women
- Women who have had children
- Women undergoing the menopause
- Women who have had a hysterectomy
- Men who have had a prostatectomy
- People with constipation
- People with dementia
- People with diabetes
- People with diarrhoea
- People with heart failure
- People with learning disabilities
- People with mental health problems
- People with musculoskeletal problems, e.g. arthritis
- People with neuropathological problems e.g. dementia, Parkinson’s disease, spina bifida, multiple sclerosis, stroke
- People who are obese
- People with spinal injury
- People with urinary tract infections (UTIs)
- Older people (65+).
A continence service needs to be person-centred and seek to help people identify their needs and agree shared goals. The person experiencing the continence issue should be an active partner in their own care and feel that they have had a good experience (NHS England, 2015). It is important that they are made aware of all the possible options for treatment and be free to choose the approach that will be most likely to meet their individual needs.
The EICC report recommends that as well as treating people with empathy and respect and ensuring that their voice is heard and responded to, a person-centred approach should include person-held records, education about how to manage their condition and prevent a deterioration in their health and, if appropriate, access to personal budgets (NHS England, 2015). People need to experience quick, efficient access to experts who can assess and diagnose the underlying condition or cause of the continence problems and offer effective treatment, self-management and, when required, referral to appropriate specialist services, e.g. urology, urogynaecology, gastroenterology, learning disabilities, neurology, paediatrics, geriatrics, specialist physiotherapy, etc.
True empowerment of people brings choice: not just a choice of provider, but choice of what they feel is appropriate for them. This may mean turning down a particular treatment option. Empowerment means having access to information, advice and treatment and brings the understanding that people have the right to continent living, whenever this is achievable. This enables an optimum quality of life, independence and personal dignity.
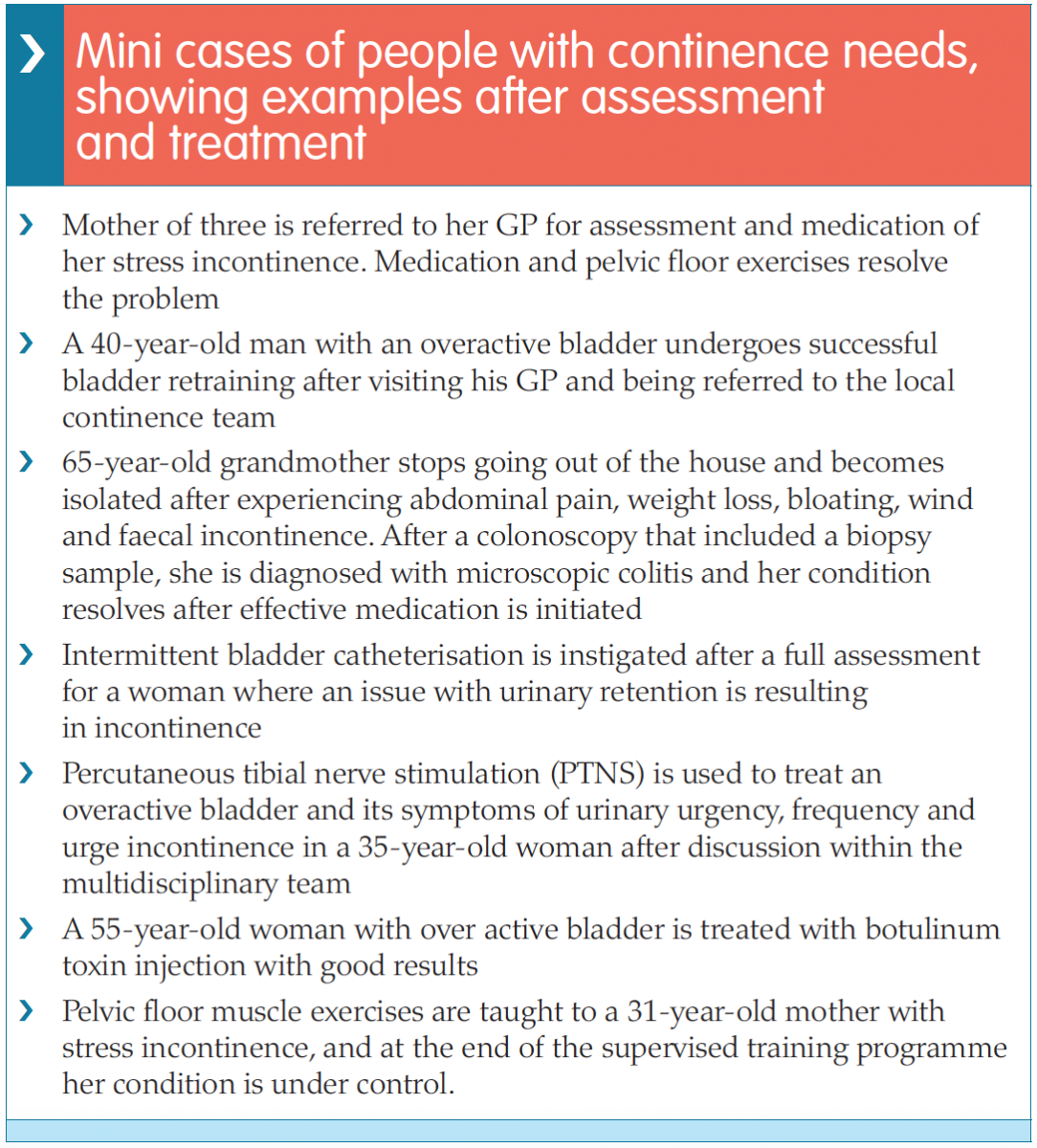
 The complexity of continence care is that the root cause is not just one problem, but a myriad of potential and often treatable conditions that span many different specialities (see Mini case examples box). Understanding this complexity and educating health and social care staff (who are most likely to have contact with individuals experiencing continence difficulties) so that they can provide an assessment which gathers the information required for appropriate management or referral pathways is the challenge that health, social and educational institutions need to achieve.
The complexity of continence care is that the root cause is not just one problem, but a myriad of potential and often treatable conditions that span many different specialities (see Mini case examples box). Understanding this complexity and educating health and social care staff (who are most likely to have contact with individuals experiencing continence difficulties) so that they can provide an assessment which gathers the information required for appropriate management or referral pathways is the challenge that health, social and educational institutions need to achieve.
The EICC report recommends that as well as treating people with empathy and respect and ensuring that their voice is heard and responded to, a person-centred approach should include person-held records, education about how to manage their condition and prevent a deterioration in their health and, if appropriate, access to personal budgets (NHS England, 2015). People need to experience quick, efficient access to experts who can assess and diagnose the underlying condition or cause of the continence problems and offer effective treatment, self-management and, when required, referral to appropriate specialist services, e.g. urology, urogynaecology, gastroenterology, learning disabilities, neurology, paediatrics, geriatrics, specialist physiotherapy, etc.
True empowerment of people brings choice: not just a choice of provider, but choice of what they feel is appropriate for them. This may mean turning down a particular treatment option. Empowerment means having access to information, advice and treatment and brings the understanding that people have the right to continent living, whenever this is achievable. This enables an optimum quality of life, independence and personal dignity.
NHS England, 2015
 The complexity of continence care is that the root cause is not just one problem, but a myriad of potential and often treatable conditions that span many different specialities (see Mini case examples box). Understanding this complexity and educating health and social care staff (who are most likely to have contact with individuals experiencing continence difficulties) so that they can provide an assessment which gathers the information required for appropriate management or referral pathways is the challenge that health, social and educational institutions need to achieve.
The complexity of continence care is that the root cause is not just one problem, but a myriad of potential and often treatable conditions that span many different specialities (see Mini case examples box). Understanding this complexity and educating health and social care staff (who are most likely to have contact with individuals experiencing continence difficulties) so that they can provide an assessment which gathers the information required for appropriate management or referral pathways is the challenge that health, social and educational institutions need to achieve.CONTAINMENT PRODUCTS
Long-term use of containment products is an option when a curable problem or diagnosis has not been found and full assessment and referral pathways explored. Containment products, such as pads, hand-held urinals, etc can help people feel comfortable and secure. However, they require regular assessment to ensure that they are the best option for each individual’s needs.Indwelling catheters are associated with significant morbidity and mortality and other options, such as teaching people intermittent self-catheterisation (ISC), need exploring (NHS England, 2015).
EDUCATION
Educating the workforce is a critical part of delivering an effective, integrated person-centred continence service. As the EICC report states:The NHS is defined by its staff: developing and supporting the workforce within a culture of safety and compassion is crucial to ensuring the best outcomes for people. The correct education and training helps us all understand the importance of the need to embrace the right skills, values and behaviours for the benefit of all those with continence needs who touch our services.
NHS England, 2015
The report goes on to emphasise that it is the responsibility of each individual member of staff to be aware of NHS England’s priorities in relation to continence services, and to identify how they can be involved in helping achieve these objectives (NHS England, 2015). It recommends education at undergraduate level for all physiotherapists, nurses and medical students, continuous professional development (CPD) for those who care for, or may be able to identify and signpost people with continence needs, and fundamental continence care education for other workers, such as care assistants, who will be involved in delivering care.
All staff that come into contact with an adult who has a bladder or bowel problem should be trained to assess, treat and refer as required. It is essential to reduce the negative impact and improve the quality of life for those with bladder and bowel care problems. The cost implication of not providing staff that are competent to proactively diagnose and treat bladder and bowel problems is significant.
UKCS, 2015
In the UKCS’s guide detailing the minimum standards for continence care, a multidisciplinary team from the UKCS provide modules detailing the knowledge and skills required to provide an effective continence care service across primary, secondary and tertiary settings. These are laid out into eight modules, each providing a simple overview of the learning and minimum standards needed to perform an assessment of, or manage a patient with continence needs:
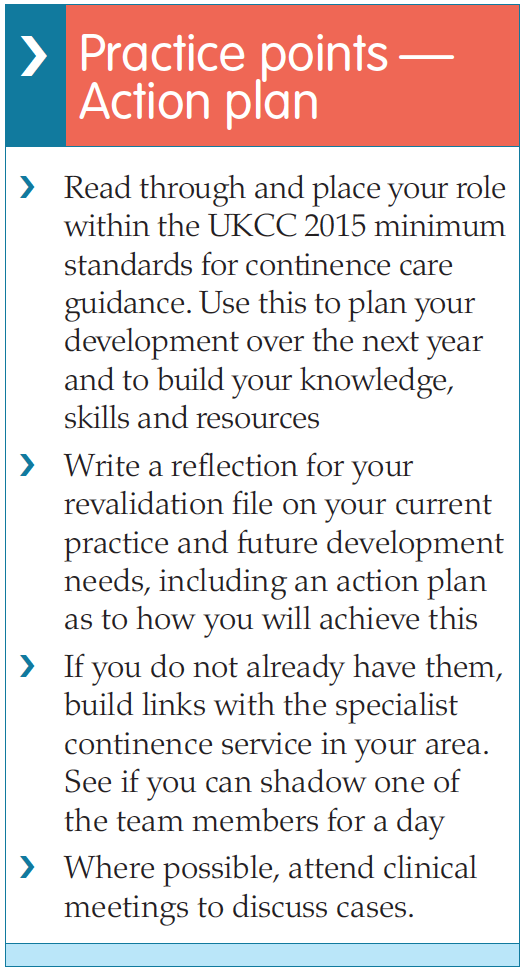
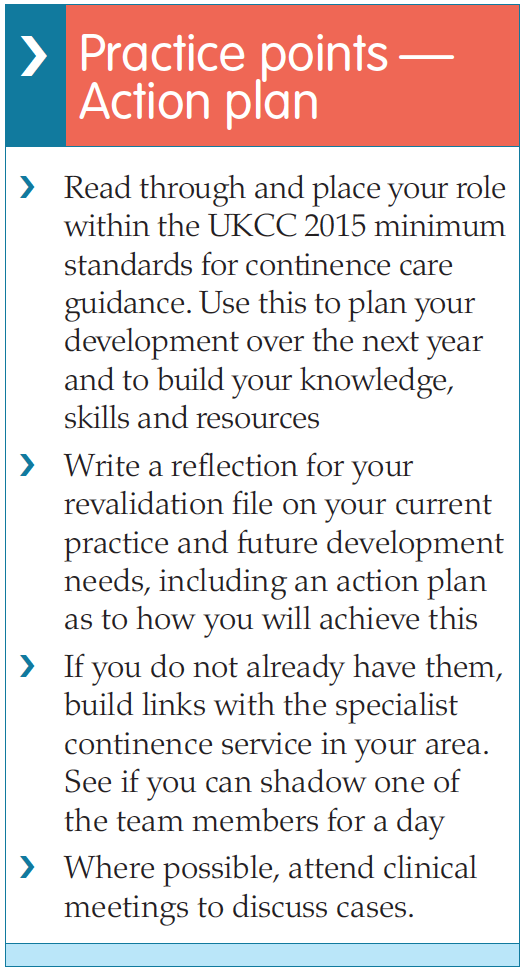
 The aim of this continence care document is not only to reduce variation in practice across the UK and ensure that all those with continence needs are seen and managed by properly trained staff, but also to improve outcomes in continence care. In addition, the document aims to facilitate the development of appropriate pre and post-registration education by service leads and educational institutions. It is hoped that e-learning packages and study days can be developed using the modules in the guide for healthcare professionals as part of their continuing professional education, and that continence care skills will be included as a mandatory part of pre-registration nurse and other relevant healthcare professional initial training. The UKCC 2015 report recommends that every healthcare professional who encounters patients with continence needs should use the document to identify where their role sits within its framework and take individual responsibility for ensuring that they have the skills and competencies required. This is part of the Nursing and Midwifery Council’s (NMC) requirements for ensuring that nurses have the competencies required to deliver care and can be included as part of reflection and revalidation (NMC, 2015).
The aim of this continence care document is not only to reduce variation in practice across the UK and ensure that all those with continence needs are seen and managed by properly trained staff, but also to improve outcomes in continence care. In addition, the document aims to facilitate the development of appropriate pre and post-registration education by service leads and educational institutions. It is hoped that e-learning packages and study days can be developed using the modules in the guide for healthcare professionals as part of their continuing professional education, and that continence care skills will be included as a mandatory part of pre-registration nurse and other relevant healthcare professional initial training. The UKCC 2015 report recommends that every healthcare professional who encounters patients with continence needs should use the document to identify where their role sits within its framework and take individual responsibility for ensuring that they have the skills and competencies required. This is part of the Nursing and Midwifery Council’s (NMC) requirements for ensuring that nurses have the competencies required to deliver care and can be included as part of reflection and revalidation (NMC, 2015).
The author, who works as a general practice nurse (GPN), is aware that a number of the patients she sees may have unspoken continence needs. Incontinence is a common problem and the UKCS 2015 report therefore recommends that it should initially be assessed in the community. The basic assessment skills required for this will include having information to give to patients about bladder/bowel function and the use of simple questions to assess this, screening questionnaires, symptom questions, bladder diaries to assess frequency and volume, as well as knowledge on how to refer patients for a bladder scan to assess postvoid residual urine when required. Understanding referral pathways to access specialist care, for example, urodynamic teams, is also important. There is a resource list at the end of this article which will be useful for educating both nurses and patients and explaining the importance of lifestyle intervention, e.g. weight loss, drinking habits as well as pelvic floor exercises, or bladder training. Taking part in an accredited training course is also important. Specialist generalists in the community should be involved with case finding, i.e. asking people the right questions within a routine holistic assessment and providing basic continence care for some, while referring others onto specialist services.
- Module 1: Structure of continence services
- Module 2: Basic assessment and conservative management of bladder and bowel symptoms
- Module 3: Specialist assessment and conservative management of the female lower urinary tract
- Module 4: Specialist assessment and conservative management of the male lower urinary tract (LUT)
- Module 5: Specialist assessment and conservative management of patients with neuropathic bladder
- Module 6: Specialist assessment and conservative management of constipation and faecal incontinence
- Module 7: Urinary catheterisation
- Module 8: Assessment tools.
 The aim of this continence care document is not only to reduce variation in practice across the UK and ensure that all those with continence needs are seen and managed by properly trained staff, but also to improve outcomes in continence care. In addition, the document aims to facilitate the development of appropriate pre and post-registration education by service leads and educational institutions. It is hoped that e-learning packages and study days can be developed using the modules in the guide for healthcare professionals as part of their continuing professional education, and that continence care skills will be included as a mandatory part of pre-registration nurse and other relevant healthcare professional initial training. The UKCC 2015 report recommends that every healthcare professional who encounters patients with continence needs should use the document to identify where their role sits within its framework and take individual responsibility for ensuring that they have the skills and competencies required. This is part of the Nursing and Midwifery Council’s (NMC) requirements for ensuring that nurses have the competencies required to deliver care and can be included as part of reflection and revalidation (NMC, 2015).
The aim of this continence care document is not only to reduce variation in practice across the UK and ensure that all those with continence needs are seen and managed by properly trained staff, but also to improve outcomes in continence care. In addition, the document aims to facilitate the development of appropriate pre and post-registration education by service leads and educational institutions. It is hoped that e-learning packages and study days can be developed using the modules in the guide for healthcare professionals as part of their continuing professional education, and that continence care skills will be included as a mandatory part of pre-registration nurse and other relevant healthcare professional initial training. The UKCC 2015 report recommends that every healthcare professional who encounters patients with continence needs should use the document to identify where their role sits within its framework and take individual responsibility for ensuring that they have the skills and competencies required. This is part of the Nursing and Midwifery Council’s (NMC) requirements for ensuring that nurses have the competencies required to deliver care and can be included as part of reflection and revalidation (NMC, 2015).The author, who works as a general practice nurse (GPN), is aware that a number of the patients she sees may have unspoken continence needs. Incontinence is a common problem and the UKCS 2015 report therefore recommends that it should initially be assessed in the community. The basic assessment skills required for this will include having information to give to patients about bladder/bowel function and the use of simple questions to assess this, screening questionnaires, symptom questions, bladder diaries to assess frequency and volume, as well as knowledge on how to refer patients for a bladder scan to assess postvoid residual urine when required. Understanding referral pathways to access specialist care, for example, urodynamic teams, is also important. There is a resource list at the end of this article which will be useful for educating both nurses and patients and explaining the importance of lifestyle intervention, e.g. weight loss, drinking habits as well as pelvic floor exercises, or bladder training. Taking part in an accredited training course is also important. Specialist generalists in the community should be involved with case finding, i.e. asking people the right questions within a routine holistic assessment and providing basic continence care for some, while referring others onto specialist services.
The following are some of the knowledge and skills needed to undertake a basic assessment and be able to offer conservative management of bladder and bowel symptoms (UKCS, 2015):
- Having knowledge of anatomy and physiology relevant to continence
- Understanding the impact of LUT and bowel symptoms on those experiencing them
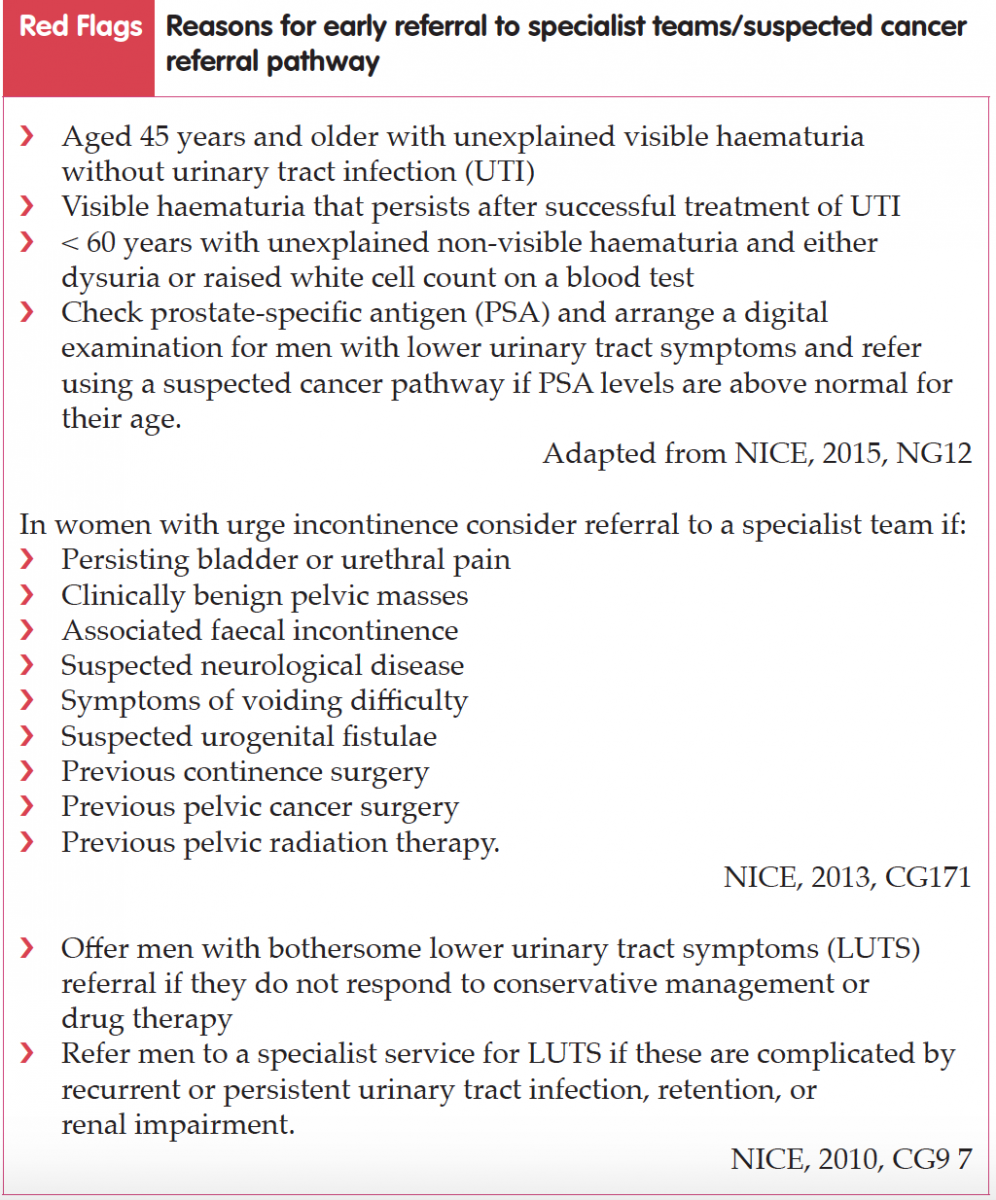
- Being able to identify red flag symptoms and when to make an urgent referral
- Understanding the conservative management of bladder and bowel symptoms
- Knowing when to refer on
- Being able to assess bladder and bowel symptoms and perform a basic clinical examination
- Thinking about other factors that can effect continence status, e.g. mobility, medications
- Being able to perform and interpret urine dipstix and know when to send a midstream urine specimen (MSU)
- Having an awareness of and access to bladder and bowel diaries
- Being aware of treatment options for continence management
- Being aware of how comorbidities can impact on bladder and bowel symptoms
- Being aware of effective lifestyle interventions, e.g. weight loss
- Having knowledge of available resources for patients
- Training must at least initially be under the supervision of an identified preceptor
Adapted from UKCS, 2015.
The author has used this list to acknowledge the current knowledge and skills she has and to plan further development within this area to fully meet the UKCS 2015 minimum standards. In her local area, NHS Education for Scotland (NES) provide an online short course entitled ‘Promotion of Continence and the Assessment of Bladder Dysfunction in Adults’ via learnPro.
In contrast, the UKCS minimum standards report recommends a specialist continence team composed of specialist nurses, specialist physiotherapists, urologists and/ or gynaecologists will be able to offer specialist assessment, advice on containment and appliances, conservative and drug management and primary surgery for uncomplicated urinary incontinence (UKCS, 2015). They will hold regular multidisciplinary team meetings and undertake audit of services. Referral to regional expert multidisciplinary teams should be available for the management of more complicated cases, e.g. women who have failed stress incontinence therapy or first-line surgery for urge urinary incontinence, people with complex neuropathy, men with post prostatectomy urinary incontinence, and people with combined urinary and faecal incontinence.
Specialist continence staff are expected to fulfil the following responsibilities (NHS England, 2015):
In contrast, the UKCS minimum standards report recommends a specialist continence team composed of specialist nurses, specialist physiotherapists, urologists and/ or gynaecologists will be able to offer specialist assessment, advice on containment and appliances, conservative and drug management and primary surgery for uncomplicated urinary incontinence (UKCS, 2015). They will hold regular multidisciplinary team meetings and undertake audit of services. Referral to regional expert multidisciplinary teams should be available for the management of more complicated cases, e.g. women who have failed stress incontinence therapy or first-line surgery for urge urinary incontinence, people with complex neuropathy, men with post prostatectomy urinary incontinence, and people with combined urinary and faecal incontinence.
Specialist continence staff are expected to fulfil the following responsibilities (NHS England, 2015):
- Provide clinical leadership of continence services › Provide advanced clinical assessment and treatment
- Advise about the design and delivery of services › Develop clinical guidelines and pathways
- Endorse best practice by teaching › Guide and correct practice where necessary
- Assess and review policies and practices: make recommendations for change
- Evaluate clinical outcomes.
CONCLUSION
Most nurses will encounter people with continence needs. Being aware of the standards guiding continence care is crucial if healthcare professionals are to meet the needs of this significant proportion of the population and ensure minimum standards for continence care are delivered. While there may be many competing demands on the topics healthcare professionals choose for continuous professional development, continence care certainly needs to be one of them.Useful resources
For impartial product advice: www.continenceproductadvisor.org
Association for Continence Advice (ACA): www.aca.uk.com
Bladder & Bowel Community: www.bladderandbowel.org
British Association of Urological Nurses (BAUN): www.baun.co.uk
ERIC (The Children’s Continence Charity): www.eric.org.uk
PromoCon Disabled Living: www.disabledliving.co.uk/ PromoCon/About
Paediatric Continence Forum: www.paediatric continenceforum.org
United Kingdom Continence Society: www.ukcs.uk.net
NHS choices: www.nhs.uk/ Conditions/Pages/Hub.aspx
NHS Inform: www.nhsinform.scot
Patient: https://patient.info
Association for Continence Advice (ACA): www.aca.uk.com
Bladder & Bowel Community: www.bladderandbowel.org
British Association of Urological Nurses (BAUN): www.baun.co.uk
ERIC (The Children’s Continence Charity): www.eric.org.uk
PromoCon Disabled Living: www.disabledliving.co.uk/ PromoCon/About
Paediatric Continence Forum: www.paediatric continenceforum.org
United Kingdom Continence Society: www.ukcs.uk.net
NHS choices: www.nhs.uk/ Conditions/Pages/Hub.aspx
NHS Inform: www.nhsinform.scot
Patient: https://patient.info
References
British Association of Urological Surgeons Limited (BAUS). Available online: www. baus.org.uk/patients/conditions/5/ incontinence_of_urine (accessed 21 January, 2018)
National Institute for Health and Care Excellence (2010) Lower urinary tract symptoms in men: management (last updated June 2015). Clinical guideline [CG97]. Available online: www.nice.org. uk/guidance/cg97
National Institute for Health and Care Excellence (2013) Urinary incontinence in women: management (last updated November 2015). Clinical guideline [CG171]. Available online: www.nice. org.uk/guidance/cg171
National Institute for Health and Care Excellence (2015) Suspected cancer: recognition and referral (last updated July 2017). NICE guideline [NG12].
Available online: www.nice.org.uk/guidance/ng12 NHS England (2014) Five year forward view. NHS England, London. Available online: www.england.nhs.uk/wpcontent/ uploads/2014/10/5yfv-web.pdf
NHS England (2015) Excellence in continence care: Practical guidance for commissioners, provider, health and social care staff and information for the public. NHS England, London. Available online: www.engalnd.nhs.uk/commisioning/wp-content/uploads/sites/12/2015/11/ EICC-guidance-final-document.pdf
Nursing and Midwifery Council (2015) The Code. NMC, London. Available online: www.nmc.org.uk/globalassets/ sitedocuments/nmc-publications/nmccode.pdf (accessed 22 January, 2018)
United Kingdom Continence Society — continence care steering group (2015) Minimum standards for continence care in the United Kingdom. Available online: www.ukcs.uk.net/wp-content/uploads/2016/04/15091716_Revised_ Min_Standards_for_CC_in_UK.pdf (accessed 21 January, 2018)
National Institute for Health and Care Excellence (2010) Lower urinary tract symptoms in men: management (last updated June 2015). Clinical guideline [CG97]. Available online: www.nice.org. uk/guidance/cg97
National Institute for Health and Care Excellence (2013) Urinary incontinence in women: management (last updated November 2015). Clinical guideline [CG171]. Available online: www.nice. org.uk/guidance/cg171
National Institute for Health and Care Excellence (2015) Suspected cancer: recognition and referral (last updated July 2017). NICE guideline [NG12].
Available online: www.nice.org.uk/guidance/ng12 NHS England (2014) Five year forward view. NHS England, London. Available online: www.england.nhs.uk/wpcontent/ uploads/2014/10/5yfv-web.pdf
NHS England (2015) Excellence in continence care: Practical guidance for commissioners, provider, health and social care staff and information for the public. NHS England, London. Available online: www.engalnd.nhs.uk/commisioning/wp-content/uploads/sites/12/2015/11/ EICC-guidance-final-document.pdf
Nursing and Midwifery Council (2015) The Code. NMC, London. Available online: www.nmc.org.uk/globalassets/ sitedocuments/nmc-publications/nmccode.pdf (accessed 22 January, 2018)
United Kingdom Continence Society — continence care steering group (2015) Minimum standards for continence care in the United Kingdom. Available online: www.ukcs.uk.net/wp-content/uploads/2016/04/15091716_Revised_ Min_Standards_for_CC_in_UK.pdf (accessed 21 January, 2018)


