Recently, I was delighted to join the Florence Nightingale Foundation to talk on this topic. This article summarises this session, but if you are curious, you can see the presentation at: https://youtu.be/u72w_7gtZQM.
Digital is a pretty major deal. I think we all know implicitly that this is the case, as, after all, the world is changing around us and more of our lives are happening on magic boxes and screens, in technologically perplexing ways. As an experience, we are consuming more digital things in different ways, which is changing how we interact with the world around us — from driving, eating, communicating with those we care about, sharing and receiving information, entertaining ourselves and meeting a future partner.
But healthcare professionals on the frontline would be entirely forgiven for asking: what exactly is digital when we talk about patient care? The landscape can be confusing and is often focused on people coming in and installing some technology, which may or may not create consequences for you and your colleagues, or just do the same thing you did before via a screen, where you may or may not be on mute.
To answer this question, let’s talk about what healthcare professionals currently do, what they want to be able to do, and what will inevitably help them to do this.
Digital is a pretty major deal. I think we all know implicitly that this is the case, as, after all, the world is changing around us and more of our lives are happening on magic boxes and screens, in technologically perplexing ways. As an experience, we are consuming more digital things in different ways, which is changing how we interact with the world around us — from driving, eating, communicating with those we care about, sharing and receiving information, entertaining ourselves and meeting a future partner.
But healthcare professionals on the frontline would be entirely forgiven for asking: what exactly is digital when we talk about patient care? The landscape can be confusing and is often focused on people coming in and installing some technology, which may or may not create consequences for you and your colleagues, or just do the same thing you did before via a screen, where you may or may not be on mute.
To answer this question, let’s talk about what healthcare professionals currently do, what they want to be able to do, and what will inevitably help them to do this.
ANALOGUE VS DIGITAL CARE
Patients are complex — even the less complex ones — and the healthcare workforce’s ability as a system to take their many needs and nuances into account is, I feel, naturally limited. Thus, approaches to holistic care need to strike a balance between a clinician’s skillset and the time they have with that patient. Every minute counts, and in a stretched NHS this can fall into a 9.2-minute slice of time (on average) (Salisbury, 2019). Everyone tries their best but is limited by the workforce equation.
Looking towards the future, a system with greater demand (ageing population), less money, and major challenges in having an adequate healthcare workforce, feels perilous. Yet, looking at the NHS ‘Long Term Plan’ (NHS England, 2019), there are also major ambitions for care, such as personalisation, place, prevention, self-care, integration — all of which should ultimately lead to better outcomes. That said, there are major challenges inherent in such ambitions, such as financial, workforce (supply), and an ageing population (demand), to be overcome. The answer is that most, if not all of this, is predicated on the hope of digital technologies; not the range of systems that clinicians often get to use, but ones that help you seamlessly navigate your family holiday, buy that black Friday purchase, or watch the next show on Netflix — i.e. that offer personalised and attractive user-centred experiences for day-to-day lives.
This means a coordinated system of collecting a great deal of relevant data, that can be used to help predict an intervention or strategy, nudging healthcare professionals and patients towards the most successful outcome (Health Education England [HEE], 2019). And, this may be less far away than expected, and change current jobs in the NHS beyond recognition.
THE REVOLUTION IS HERE, AND COMING TO A PATIENT NEAR YOU
Revolution is an overused term, but as a society most leading voices agree that we are entering the second machine age, where as was the case with technology replacing the need for physical human power, we will now start to see machines automating the cognitive work that humans do, the tasks and analytical decisions that fill our day, including many forms of day-to-day communication. This new form of power, put simply, will be enabled by different forms of artificial intelligence (AI) that will get ever-more sophisticated. This is already happening in many industries which you use to buy things, such as travel or simply getting a pizza delivered, and will inevitably reshape health and social care in the 2020s (HEE, 2019).
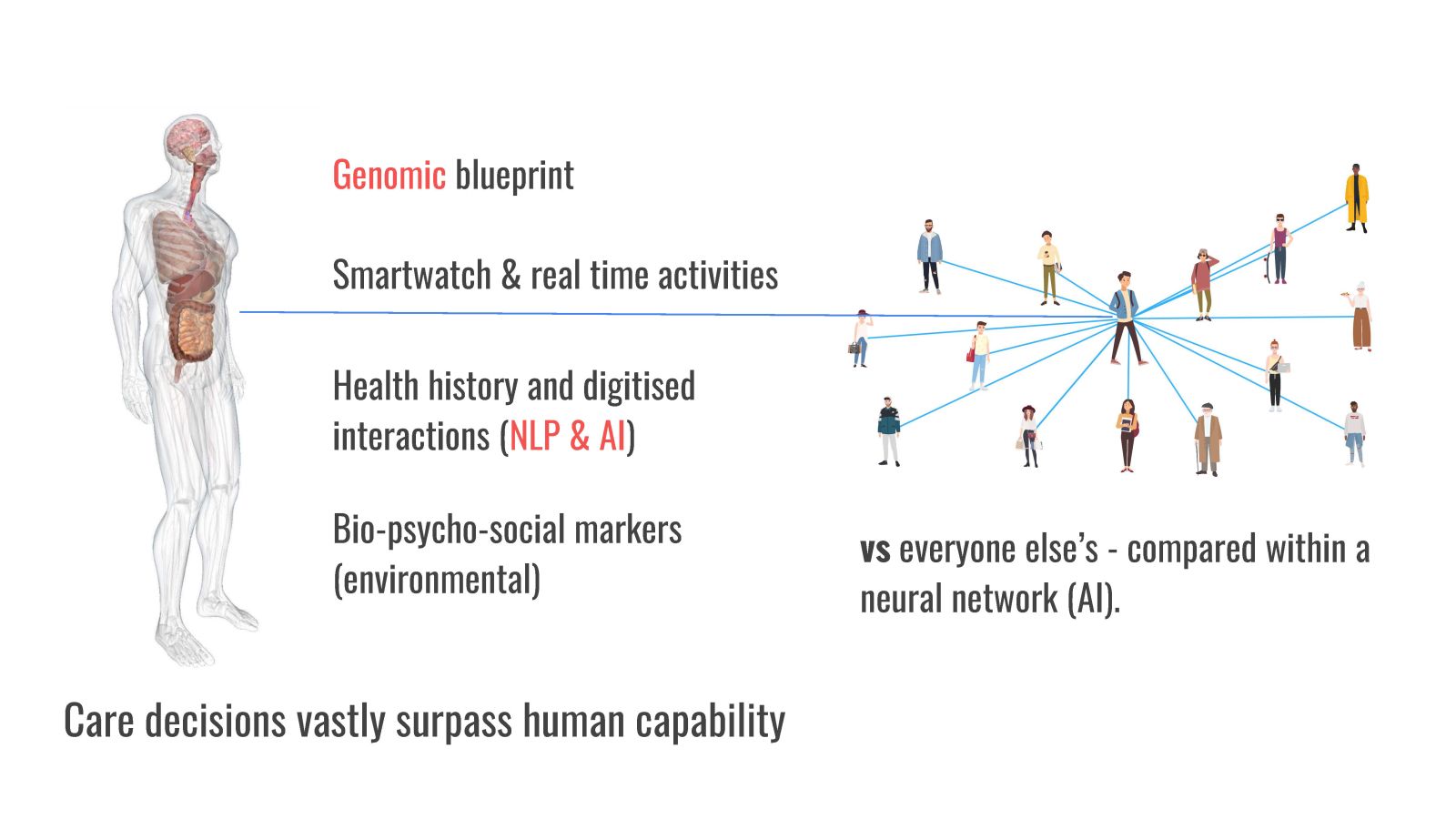
It begins with data. In the Topol Review commissioned by Health Education England (HEE, 2019), a number of notable technologies are identified: from wearables and devices to virtual interactions, to the millions of consistent and comparable data points on a person that will be able to be seen through genomic profiling, to smartphones, robotics and image, video and voice/language recognition and processing. I could write an article on each of these, but the point is that all of them are collectors and/or translators of incredible amounts of data that could be relevant to current, and possible future care needs.
Through this data, there are trends in our day-to-day lives, our individual blueprints, or lifestyle, bio-psychosocial factors, our feelings, tone of voice, and, of course, useful health signs, such as blood glucose or respiratory rate. Arguably, it could be the secret key to stopping life-limiting or ending health events from happening, or the answer to how we should respond when they do. It is also more data than we could even begin to comprehend and do something meaningful with, regardless of the amount of time we would have to work through it.
But very fast computers running different forms of algorithms could handle this: not just flagging up meaningful things, but potentially comparing parts of this data against millions of other people (through what is called digital twins), suggesting what may or should happen to drive a better outcome and learning and progressing all the time to improve and refine mathematical models on real-time care strategies.
What is described above is the beginning of not just a major new role in what technology is doing in care decisions, but in asking what a care decision or intervention really is, when it should happen, and what the role of a human being should be in contributing to it. It might currently seem incomprehensible that we would shift our trust away from a nurse or doctor when it comes to diagnosis or treatment strategies, after all for life and death decisions. However culturally, we can see this shift happening as our trust moves from the A-to-Z to Google’s navigation algorithms to that of a self-driving car. Maybe one day soon, a human driving a car might seem like an unnecessarily dangerous endeavour, and perhaps the same concern could be the case about a human providing health advice independent of algorithms.
HUMAN CARE 2.0
While this might feel like a daunting and uncertain future for healthcare professionals, surely what we all just want for ourselves, our loved ones and patients, is the best possible care. Ultimately, as a (very infrequent) patient, I want two things from the care system: to support me in living healthily — giving me the right advice, support and care provision — and to offer me a system of humanity as I progress through my life, and ultimately towards its end.
A revolution in technologically driven care may offer the first objective, and in unimaginable ways, but I cannot see how a system of humanity and care will ever be meaningfully replaced by technology. To ensure that a care system of both technology and humanity is developed in the years ahead, we will need the frontline healthcare workforce not only to understand and embrace technology, but also to participate and lead in this digital transition.
To find out more…
Sector 3 Digital runs programmes around digital and provides advice and support to frontline health and social care organisations, national bodies, and healthtech companies.
You can follow Liam on:
LinkedIn (www.linkedin.com/in/liam-d-cahill/)
Twitter @Liamsdigital
Website: www.sectorthree.tech/who/
Liam Cahill is the founder of Sector 3 Digital.
References
Health Education England (2019) The Topol Review. Preparing the healthcare workforce to deliver the digital future. Available online: https://topol.hee.nhs.uk/
NHS England (2019) NHS Long Term Plan. Available online: www.longtermplan.nhs.uk/
Salisbury H (2019) The 10 minute appointment. BMJ 2019: 365:I2389
NHS England (2019) NHS Long Term Plan. Available online: www.longtermplan.nhs.uk/
Salisbury H (2019) The 10 minute appointment. BMJ 2019: 365:I2389
This piece was first published in the Journal of General Practice Nursing. To cite this article use: Cahill L (2022) What does the future of digital hold for the clinical workforce? J Gen Pract Nurs 8(1): 16–17


