Indwelling urinary urethral or suprapubic catheterisation is regularly employed post operatively on urology and urogynaecology wards to manage urinary retention. However, urinary catheters are indicated for other reasons, which are outlined in the HOUDINI box in Figure 1.
Urinary catheterisation is an invasive procedure that should be avoided, but if it cannot be, then it should be removed as soon as possible to prevent the unwanted complications described above. Indeed, the length of time a catheter is left in situ has direct implications on the increased risk of developing an infection (Holroyd, 2020). The acronym HOUDINI (as in make it disappear) was developed to enable staff to recognise indications for continued catheter use. The catheter should be removed if it does not follow the indications illustrated in Figure 1.
Catheter care bundles should be implemented to help reduce the incidence of CAUTI, underpinned by HOUDINI principles, a protocol for management of catheterised patients, use of which is now widespread (Adams et al, 2012). HOUDINI principles require a daily review of ward-based patients to reassess the need for the catheter and to determine when it can be removed.
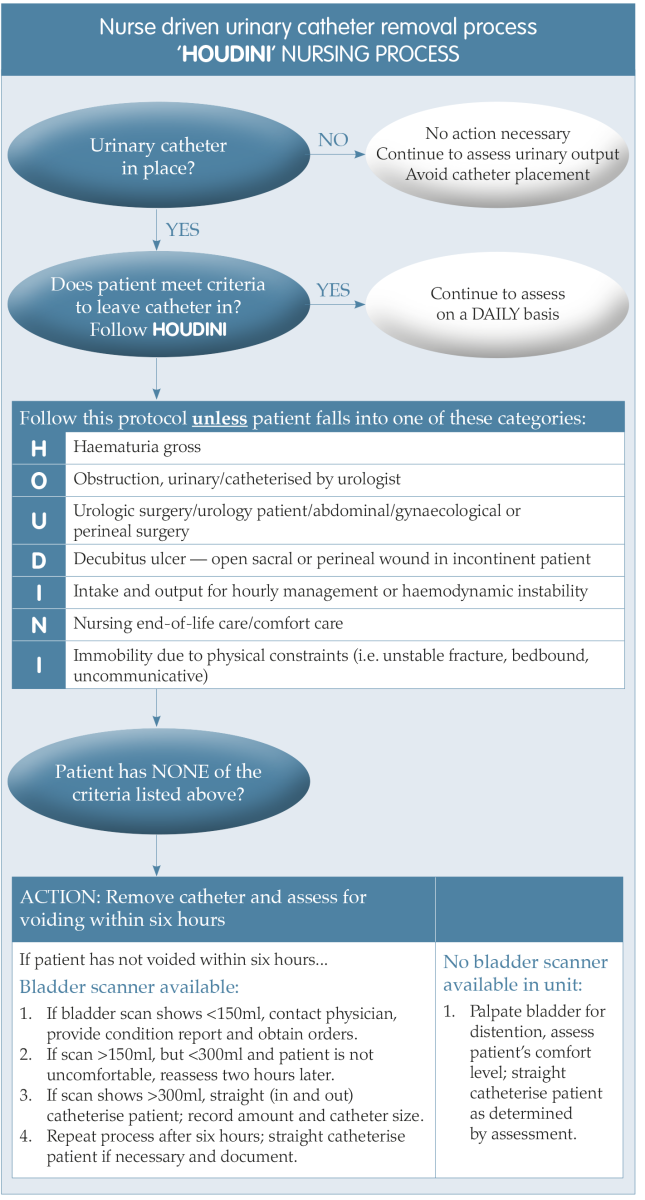
Figure 1. A nurse driven process for timely removal of urinary catheters (Yatim et al, 2016).
WHAT IS A TWOC?
The primary aim of TWOC is to establish the ability effectively and successfully to empty the bladder (Robinson, 2005). It involves removal of the catheter followed by monitoring of urinary output to ensure the bladder is voiding completely. The removal of an indwelling catheter is a relatively simple procedure, and, in the authors’ clinical experience, most TWOCs are successful. A failed TWOC is determined when a patient fails to void fully, resulting in a need to recatheterise. When a second attempt fails, they will require referral to a urologist for opinion/treatment. It is recommended that clinicians refer to the local TWOC protocol for guidance and local referral pathway (Holroyd, 2020).
HOSPITAL OUTPATIENT TWOC — RATIONALE FOR CHANGE
In the authors’ organisation, TWOCs have been carried out in hospital outpatient departments, involving the patient staying all day and often having to travel over 45 minutes in hospital transport to reach the department. Where a TWOC is carried out may have a bearing on the success of the outcome (Holroyd, 2020). The pressure to void in a strange and clinical environment can exacerbate anxiety, whereas a TWOC at home is less pressurised and thus more conducive to a successful outcome (Warrilow et al, 2004). According to Warrilow et al (2004), when patients were given options, they chose a TWOC at home.
The authors of this paper identified through catheter-related clinical incident reporting that there were significant delays with hospital TWOC appointments. Then, in 2000, the Covid-19 pandemic further affected access for patients when the local urology-based TWOC clinic was temporarily suspended.
A deep dive review highlighted that the TWOC appointment requests came from all wards and directorates within the organisation and were sent by a ward doctor directly to the urology department requesting a hospital TWOC appointment. It is not clear why more TWOCs are not routinely attempted before discharge, possibly due to the pressure for hospital beds and the need to expedite discharge. The referrals for a TWOC were either faxed or posted to urology by the ward doctor, but some were lost in the system, resulting in patients failing to receive an appointment. The urology department who processed the referral required a urologist to triage it and pass on to the urology nurses, and then on to clerical staff to send the outpatient appointment.
High demand for TWOC combined with limited capacity in urology and compounded by lack of information on discharge meant that patients waited 8–12 weeks or more for a TWOC appointment.
This excessive wait was first identified from catheter-related clinical incidents and root cause analysis (RCA) review by the authors. Once identified, these concerns were escalated to urology management as the delay in removing the urinary catheters posed unnecessary risk to patients from CAUTI and other complications, such as catheter non-draining, recurrent blockage or urethral erosion. Furthermore, the patients were told on discharge that they would receive an appointment for TWOC in two weeks. Going home with a catheter is stressful and when the two-week timescales were not met, patients became more anxious.
CATHETER-RELATED CLINICAL INCIDENT REPORTING AND ROOT CAUSE ANALYSIS
Many types of clinical incidents can be addressed through RCA and, as catheters and omissions in catheter care can cause significant harm, the process of RCA was adopted by the authors to address omissions, errors and deviations in catheter management, including the process for hospital discharge. Table 1 illustrates the RCA process.
For the past four years, the authors’ health board has been working to reduce catheter-related incidents and harm and to implement a discharge pathway to improve the process for a patient going home with a catheter. The aim has been hospital avoidance, an important strategy for the organisation to reduce emergency department pressures. If a patient is not discharged appropriately as per the pathway, readmission is often the result to deal with an emergency catheter-related issue.
.png)
Table 1. Root cause analysis process (adapted from National Patient Safety Agency, 2004)
- No referral to district nurse was arranged
- No catheter or catheter bags/ fixation straps given to take home
- Poor fixation of the catheters resulted in trauma pressure damage to the urethral meatus/penis
- No referral made to the appliance service for prescribing of catheter/ drainage bags/equipment at home
- Inadequate documentation supplied for community nurses/no catheter passport supplied
- A catheter discharge pathway was not followed
- Catheter care bundles not followed or implemented
- A short-term catheter was in situ instead of a long term
- In some cases, minimal or no patient/carer education was offered on how to care for the catheter and drainage bags
- No referral for TWOC appointment or a catheter change
- Delayed TWOC appointment.
LEADING CHANGE
Clinical leadership and strategic action were called for to address these widespread organisational issues to improve patient safety and experience. First, a urinary indwelling catheter passport was implemented to improve documentation and patient education and a catheter discharge pathway was circulated. Consultant nurses in infection prevention, bladder and bowel nursing joined forces to establish a new RCA review approach to catheter-related clinical incidents for investigating and sharing the lessons learned to prevent further incidents. Through this review process, it became apparent that there were unacceptable delays for TWOC appointments. Subsequently, an action plan was developed to address the problems identified. Figure 2 shows the development stages and timescales.
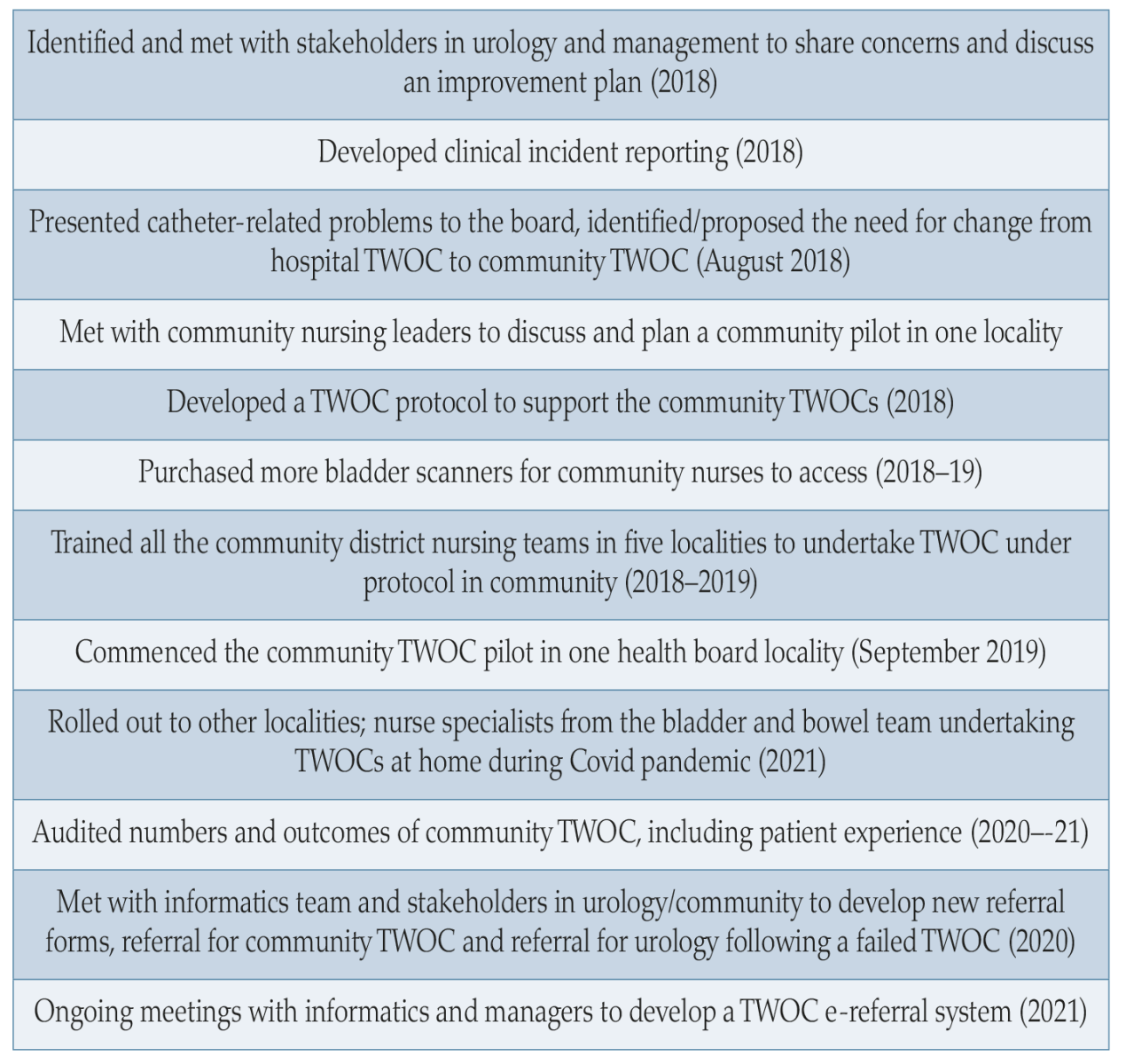
Figure 2. Service development stages and timescales.
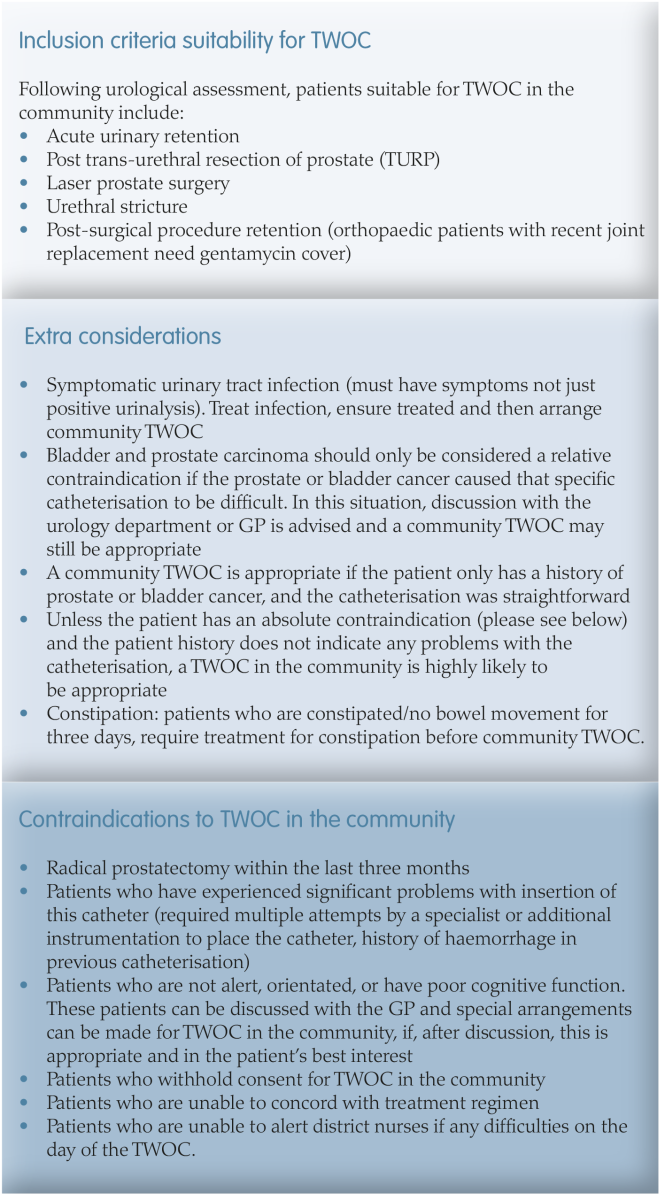
Figure 3. Inclusion and exclusion criteria.
SUPPORTING COMMUNITY NURSE-LED TWOC
A new protocol was developed to guide and support community nurses to undertake TWOC safely in patients’ homes. This protocol clarified inclusion and exclusion criteria for those eligible for a TWOC at home to prevent all the appointments taking place in hospital (Figure 3). More bladder scanners were purchased and made accessible for district nurses to support this new community development and adhere to the protocol.
Two new TWOC referral forms were developed and implemented to facilitate the referral process — a community TWOC referral and a urology opinion referral form. The paper referral was replaced with a new email one, however aspects of MDT e-referral process are still under development.
In September 2019, using the new TWOC protocol, a pilot was started in one locality with the district nurses undertaking TWOCs at home. The TWOC appointment was offered within a week of discharge from hospital — as opposed to waiting 8–12 weeks — considerably expediting the time to appointment.
STAKEHOLDER ENGAGEMENT
COMMUNITY TWOC PILOT AND THE ROLL OUT
The pilot started in one locality within the health board and subsequently rolled out across the other four once training in TWOC had been delivered to the community nurses. It is recommended that trained and experienced healthcare professionals who can monitor and determine the success of the procedure are available to undertake TWOCs guided by a clear followup protocol (Gilbert, 2006 cited in Holroyd, 2020).
Audit results
The pilot was audited to monitor the number of TWOCs undertaken and clinical outcomes. The project incorporated user involvement and participation, which is important in understanding patient experiences and developing services. Audit data was collected and analysed between April 2020 and March 2021:
- 276 patients referred to bladder and bowel service for a TWOC:
○ Average age 75.5 years
○ Average length of wait for TWOC — five weeks - 62% (182) patients had a community TWOC
- Reasons for not undergoing community TWOC:
○ RIP
○ Declined
○ Previously TWOCed by urology/district nurse
○ Inappropriate referral.
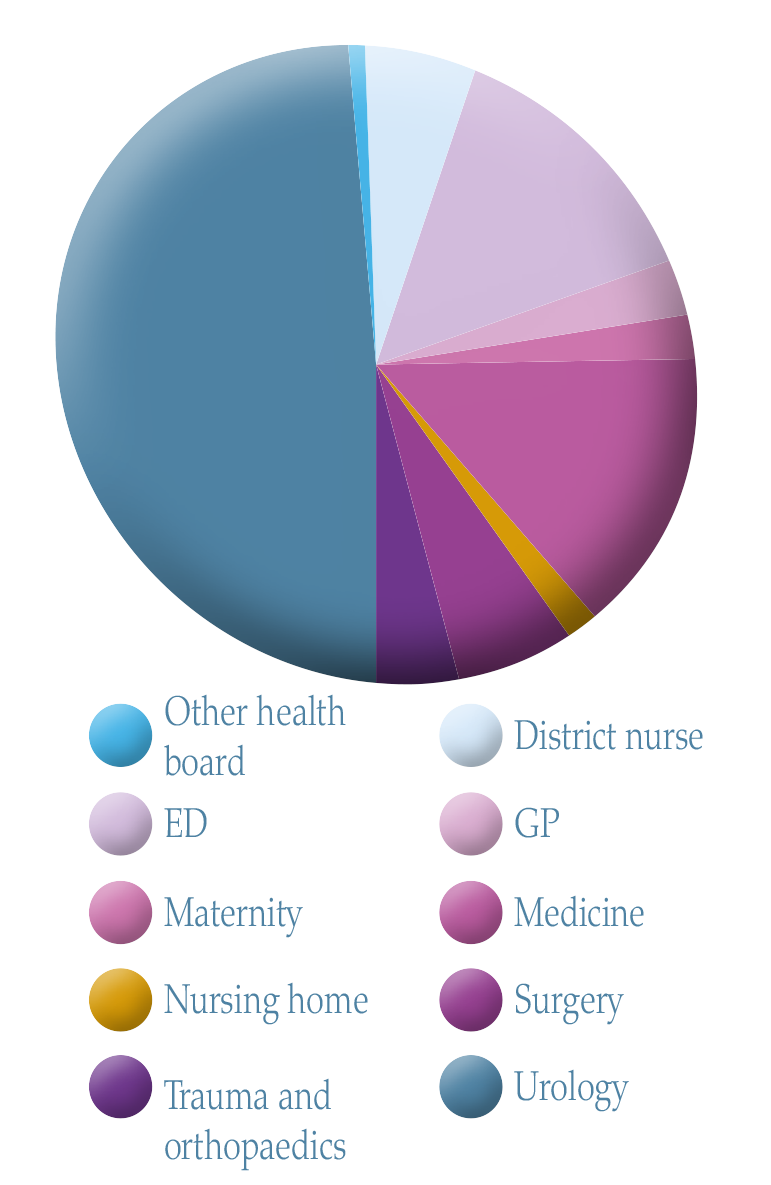
Figure 5. Referral source.
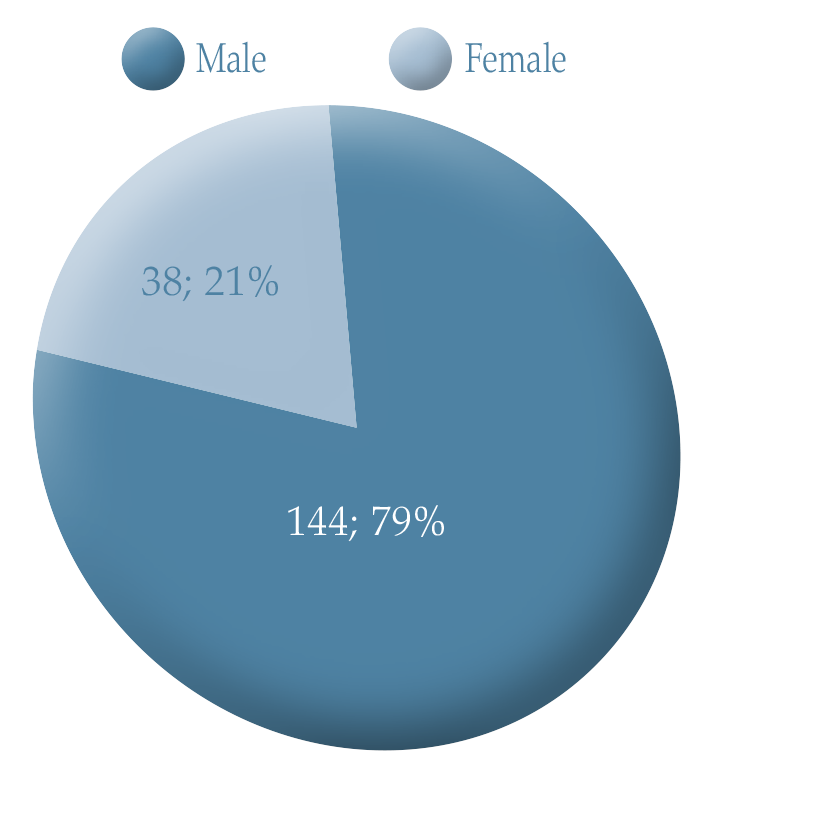
Figure 4. Gender breakdown of participants in the pilot community TWOC.
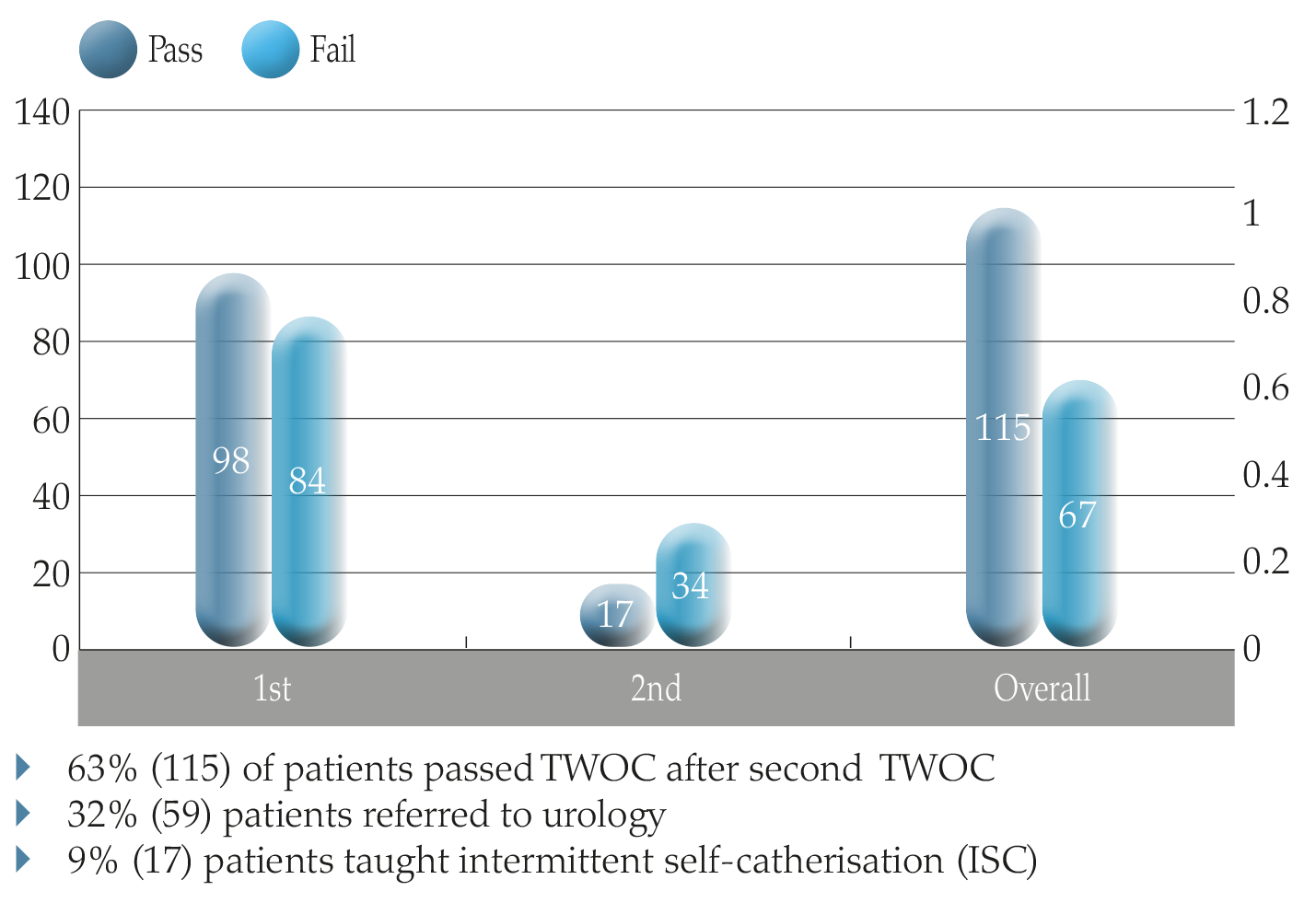
Figure 6. Outcomes of pilot TWOC in the community.
Patient experience survey
An important component of the audit undertaken between April 2020 and March 2021 was to measure patient satisfaction with having a TWOC at home by community nurses. The nurses gave the patients a survey form to complete after the TWOC was completed and these forms were forwarded to the authors to collate the information. Twenty-five patients were invited to complete the survey and 13 (52%) provided feedback (Table 2).
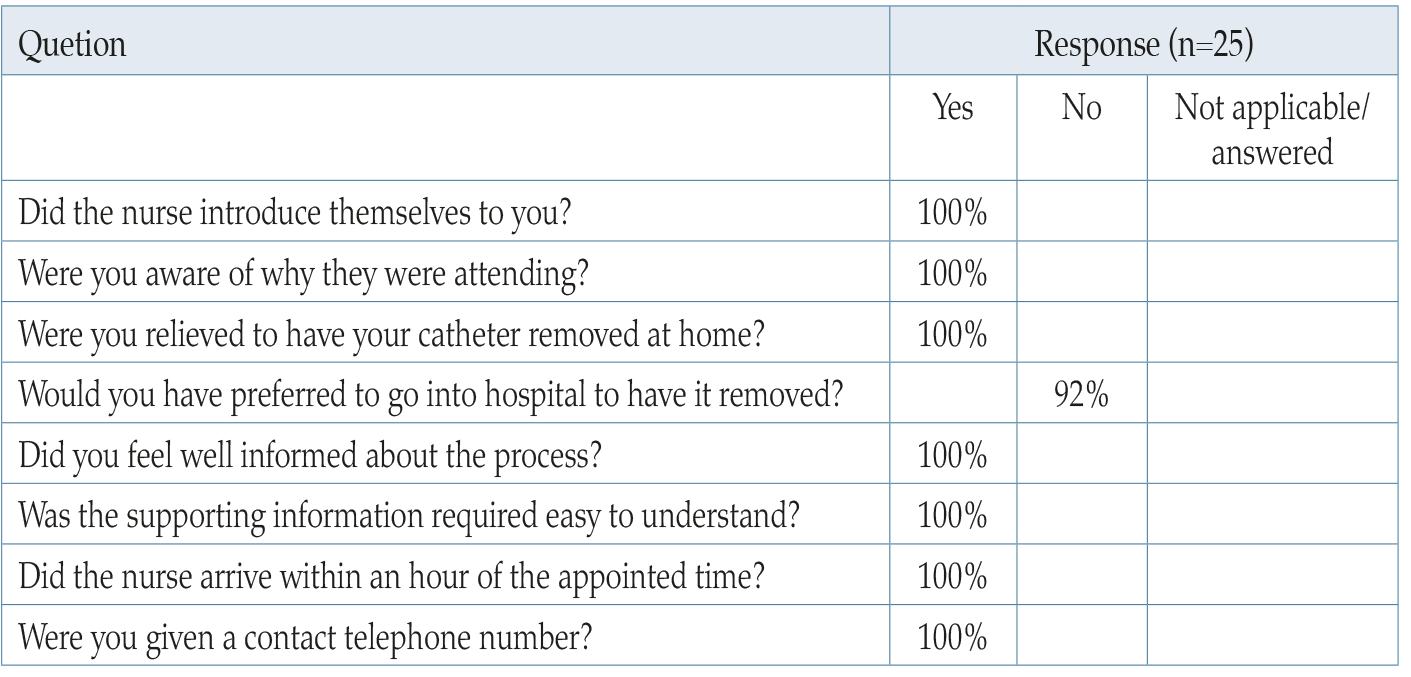
Table 2. Patient experience survey.
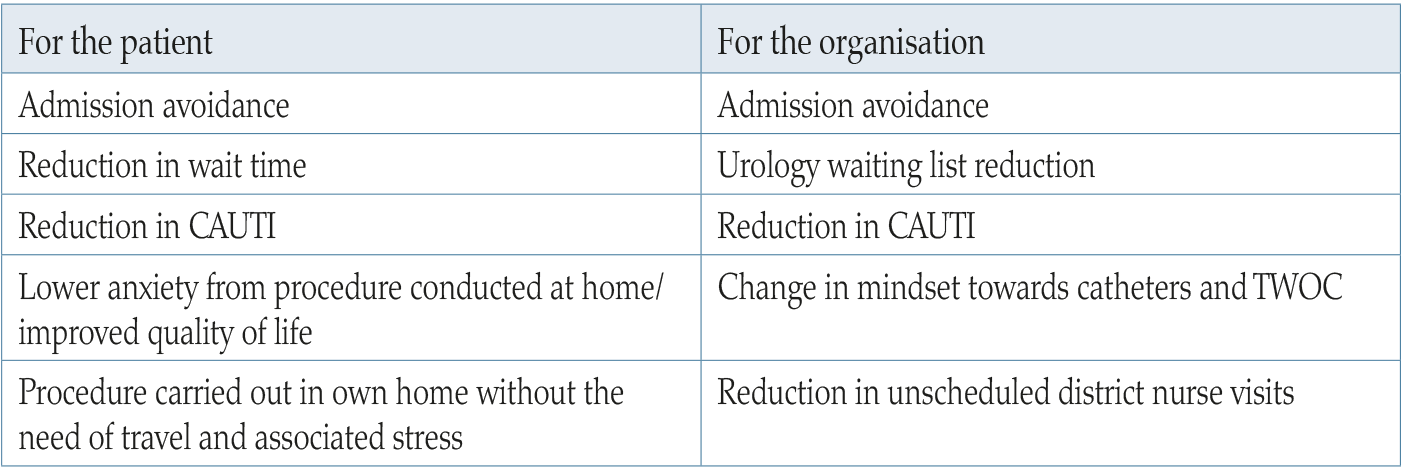
Table 3. Benefits.
- Reduction in waiting time for TWOC appointments
- Hospital admission avoidance
- Appropriateness of referral to urology/reduce urology waiting times
- Reduce prevalence of indwelling catheters in the prevention of CAUTI and other catheter-related complications
- Patient experiences of TWOC at home
- Empowerment of district nurses to undertake TWOC at home, improving catheterisation skills.
Patient comments:
Much better at home.
Staff very professional.
Nursing staff did everything and were very kind.
We found the nurses very friendly and helpful.
Nurses were excellent, very patient with my husband and so friendly, can’t thank them enough.
Staff were brilliant.
Staff kind and very efficient — did a first-class job.
Everything has been A1 could not have been better.
Very helpful and explained everything clearly.
Everything went smoothly and I was very pleased with the service.
Thank you very much for all you did.
DISCUSSION
Indwelling urinary catheters are potentially risky devices and have adverse effects on the health and social wellbeing of individuals, as well as financial implications for services (Holroyd, 2020). The links between urinary catheter use and CAUTI has been well established (Dawson et al, 2016). The literature around general catheter complications, including the numbers of catheter-related clinical incidents reported, highlights the need to reduce harm and improve management of catheterised patients. RCA can aid the development of patient-centred models of care and the scrutiny of how working practices of nurses and medical staff affect patient safety. If a particular practice does not guarantee patient safety, it should be changed (Mengis and Nicolini, 2010). The authors found that the RCA process was a useful aid in identifying what aspects of catheter management needed to change. Without this new reporting system and the RCA process, delays for TWOC appointments would remain undetected. It also alerted the authors to the fact that patients were being unnecessarily exposed to infection risks with catheters being left in situ for too long.
In the authors’ clinical opinion, working across multidiscipline/interdepartments in a large complex NHS organisation, serving a population of 600,000 across many hospital sites, has been challenging. However, the considerable investment in time and effort was worthwhile. The benefits to the patient and organisation in hospital avoidance have been made clear. The director of nursing and board have regularly been appraised of this collaborative project and shown support and enthusiasm, which has contributed to the success.
There were obvious benefits to urology, i.e. reduction of hospital TWOCs and more appropriate referrals. Patient experience was also improved as waiting times were reduced for the TWOC, thus alleviating anxiety associated with hospital attendance, especially during the Covid-19 pandemic. The benefits to community nurse teams may be less obvious but equally important. Evidence suggests that managing the longterm catheterised patient takes up significant time for district nurses and they struggle to manage unscheduled home visits caused by catheter-related complications (Pearson, 2018). By undertaking a TWOC sooner, community nurses can remove these high maintenance catheter patients from caseloads.
This transformation from hospital to community TWOC is not a new concept and other health organisations have developed and described clinical improvement projects to address this problem (Warrilow et al, 2004; Cavanagh, 2018; Nazarko, 2020). Warrilow et al (2004) showed that patients using a community care model have a more positive rating and that there are further benefits, such as freeing up beds, improving costs, reducing infection rates and seamless services. Government strategy also supports this kind of service development. However, Nazarko (2020) warns that community-based TWOC can be time intensive and that community nursing and bladder and bowel nursing services (continence services) in many parts of the UK are under pressure from cost efficiencies. Therefore, it is important that these community nurse-led services are well resourced (Tay et al, 2016) if they are to successfully transform and develop a hospital avoidance strategy.
Government strategy (A healthier Wales, 2021) sets out a long-term plan for shifting services out of hospitals to communities. This will include helping people manage their own health and long-term illnesses, making it easier for them to remain active and independent in their homes and communities. In other words, developing services that are seamless, delivered closer to home so that people only go to hospital when it is essential. This project goes some way to meet this important new agenda.
CONCLUSION
TWOC carried out in community settings is effective, evidence-based and can reduce pressures on acute hospitals. This article has described how the authors moved away from a fragmented system, which led to delays for patients, towards a timely nurse-led community TWOC service. Developing a multi-agency integrated approach between hospital and community by reorganising resources, facilitated by a strategic vision and a systematic approach to change, has resulted in a successful community nurseled TWOC service with minimum financial investment. This kind of integrated approach to delivering care enables patients to gain access to appropriate services in the right place and reduces referral and length of waits in secondary care. This is also an example of how nursing leadership can facilitate a model of organisational reform, delivering shared care that utilises the strengths of both community and secondary care working in partnership. Future initiatives will involve a drive to encourage TWOC before discharge and address the barriers in the electronic referral process between hospitals and community nursing.
References
Adams D, Bucior H, Day G, Rimmer J (2012) HOUDINI: Make that urinary catheter disappear — nurse-led protocol. J Infect Prevent 13(2): 44–46
Cavanagh C (2018) Introducing a referral pathway and proforma for trial without catheter. Br J Nurs 27(Sup6): S8–S9
Colemeadow J, Hasheim T, Batura D (2018) Trial without catheter. Br J Hosp Med 79(3): C42–C44
Dawson C, Gallo M, Prevc K (2017) TWOC around the clock: a multimodal approach to improving catheter care. J Infect Prevent 18(2): 57–64
Elwell R (2015) Developing a nurseled integrated ‘red legs’ service. Br J Community Nurs 19(1): 12, 14–19
Feneley R, Hopley I, Wells P (2015) Urinary catheters: history, current status, adverse events and research agenda. J Med Eng Technol 39(8): 459–70
Gage H, Avery M, Flannery C, Williams P, Fader M (2017) Community prevalence of long term urinary catheters use in England. Neurourol Urodyn 36(2): 293–6
Harvard (2014) cited in Colemeadow J (2018) Trial without catheter. Br J Hosp Med 79(3)
A healthier Wales: long term plan for health and social care (2021) Available online: https://gov.wales/healthier-wales-long-term-plan-health-and-social-care
Heavens K (2018) Trial without catheter referral pathways: Using district nursing services. Br J Nurs 27(sup6)
Holroyd S (2020) Trial without catheter; what is best practice? J Community Nurs 34(2): 60–7
Loveday HP, Wilson JA, Pratt RJ, et al (2014) epic 3: epic3: national evidencebased guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 86(Suppl 1): S1–70
Mengis J, Nicolini D (2010) Root cause analysis in clinical adverse events. Nurs Manag 16(9): 16–20
National Patient Safety Agency (2004) Root cause analysis toolkit. Cited in Mengis J, Davide N (2010) Root cause analysis in clinical adverse events. Nurs Manag 16(9): 16–20
Nazarko L (2020) Trial without catheters in community setting. Independent Nurse 11: 18–22
Pearson L (2018) Reducing the local use of indwelling urinary catheters in Wolverhampton. Br J Nurs 27(Sup6): S10–S11
Reid S, Brocksom J, Hamid R, et al (2021) British Association of Urological Surgeons (BAUS) and Nurses (BAUN) consensus document: management of the complications of long-term indwelling catheters. BJU Int 128: 667–77
Robinson J (2005) Removing indwelling catheters: trial without catheter in the community. Br J Community Nurs 10(12): 553–7
Tay IJ, Lyons H, Karrouze I, Taylor C, Khan AH, Thompson PM (2016) Impact of the lack of community catheter care services on the emergency department. BJU Int 118(2): 32734
Warrilow M, Williams D, Guest J (2004) The introduction of a trial without catheter model in primary care. Br J Nurs 13(17): 1035–40
Yatim J ,Wong K, Ling M, Tan K, Hockenberry M (2016) A nurse-driven process for timely removal of urinary catheters. Int J Urol Nurs 10(3): 167–72
This piece was first published in the Journal of Community Nursing. To cite this article use: Logan K, Coghlan V (2022) Transforming trial without catheter service provision. J Community Nurs 36(3): 43-50


