References
Bo K, Frawley H, Haylen B, Abarmov Y, Almeida F, Bergmans B, et al (2017) International Urogynaecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and non-pharmacological management of female pelvic floor dysfunction: Terminology for Female Pelvic Floor Dysfunction. Int Urogynaecology J 28(2): 191–213
Brucker B, Lee, R, Newman K (2020) Optimizing nonsurgical treatments of overactive bladder in the United States. Urology 145: 52–9
Bulchandani S, Tooz-Hobson P, Verghese T, et al (2014) Does vaginal oestrogen treatment with support pessaries in vaginal prolapse reduce complications? Post Reprod Health 21(4): 141–5
Chung S, Kim W (2018) Various approaches and treatments for pelvic organ prolapse in women. J Menopausal Med 24: 155–62
Dhaliwal P, Wagg A (2016) Overactive bladder: strategies to ensure treatment compliance and adherence. Clin Interv Aging 11: 755–60
DeMaagd G, Davenport T (2012) Management of urinary incontinence. PT 37(6): 345-621
Dicker D, Alfadda A, Coutinho W, et al (2021) Patient motivation to lose weight: importance of healthcare professional support, goals and self-efficacy. Eur J Internal Med 91: 10–16
Domoney C (2014) Treatment of vaginal atrophy. Women’s Health 10(2): 191–200
Dwyer L, Stewart E, Rajai A (2021) A service evaluation to determine where and who delivers pessary care in the UK. Int J Urogynaecol 32(4): 1001–6
Faiena I, Patel N, Parihar JS, et al (2015) Conservative management of urinary incontinence in women. Rev Urol 17(3): 129–39
Fontaine C, Papworth E, Pascoe J (2021) Update on the management of overactive bladder. Ther Adv Urol 13: 17562872211
International Continence Society (2018) Stress Urinary Incontinence. Available online: www.ics.org/committees/standardisation/terminologydiscussions/sui
Jones K, Harmanli O (2010) Pessary use in pelvic organ prolapse and urinary incontinence. Rev Obstet Gynecol 3(1): 3–9
Mazur-Bialy A, Kolomanska-Bogucka D, Nowakowski C, Tim S (2020) Urinary incontinence in women: modern methods of physiotherapy as a support for surgical treatment or independent therapy. J Clin Med 9(4): 1211
NHS (2022) The NHS Digital Weight Management Programme. Available online: www.england.nhs.uk/digital-weightmanagement/
National Institute for Health and Care Excellence (2013) Urinary incontinence in women: management. CG171. NICE, London. Available online: www.nice.org.uk/guidance/cg171
National Institute for Health and Care Excellence (2017) Urinary Incontinence in Women: management clinical guideline. NICE, London. Available online: www.nice.org.uk/guidance/cg171
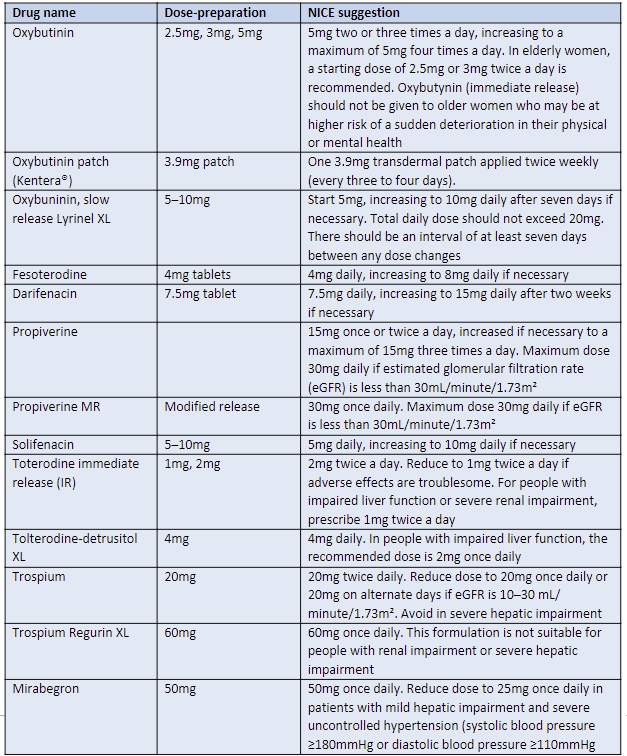
National Institute for Health and Care Excellence (2019a) Incontinence: urinary, in women; Antimuscarinics. NICE, London. Available online: https://cks.nice.org.uk/topics/incontinence-urinary-in-women/prescribing-information/antimuscarinics/
National Institute for Health and Care Excellence (2019b) Urinary incontinence and pelvic organ prolapse in women: management. NICE guideline [NG123]. NICE, London. Available online: www.nice.org.uk/guidance/ng123
National Institure for Health and Care Excellence (2021) Pelvic floor dysfunction: prevention and non-surgical management. NICE guideline [NG210]. NICE, London. Available online: www.nice.org.uk/guidance/ng210
National Institute for Health and Care Excellence/BNF (2022) Antimuscarinics (systemic). Available online: https://bnf.nice.org.uk/drug-class/antimuscarinicssystemic.html
National Institute for Health and Care Excellence/BNF (2022) Duloxetine. Available online: https://bnf.nice.org.uk/drug/duloxetine.html
Noble N (2018) Female urinary incontinence: pharmacological treatments. Nurse Prescribing 16(3): 116–20
Okeahialam N, Dworzynski K, Jacklin P, et al (2022) Prevention and non-surgical management of pelvic floor dysfunction: summary of NICE Guidelines. BMJ 376: n3049
Ostle Z (2016) Assessment, diagnosis and treatment of urinary incontinence in women. Br J Nurs 25(2): 84–91
Pomian A, Lisik W, Kosieradzki M (2016) Obesity and pelvic floor disorders: a review of the literature. Med Sci Monit 22: 1880–6
Rantell A (2015) Understanding urinary incontinence in women. Practice Nursing 26(6): 275–81
Sudol N, Adams-Piper E, Perry R, Lane F, Chen K (2019) In search of mobile applications for patients with pelvic floor disorders. Female Pelvic Med Reconstr 25(3): 252–6
Stewart E (2019) Urogynaecology. In: Holloway D, ed. Nursing management of women’s health: A guide for nurse specialists and practitioners. Springer: 215–34
United Kingdom Continence Society. UK Clinical Guideline: for best practice in the use of vaginal pessaries for pelvic organ prolapse (launched March 20221). Available online: www.ukcs.uk.net/UK-PessaryGuideline-2021
Vanichtantikul A, Tharavichitkul E, Chitapanarux I, Chinthakanan O (2017) Treatment of endometrial cancer in association with pelvic organ prolapse. Case Rep Obstet Gynecol 2017: 1640614
Zeiger B, Da Silva Carramao S, Del Roy C, et al (2021) Vaginal pessary in advanced pelvic organ prolapse: impact on quality of life. Int Urogynaecol J Nov 6: 1–8
Brucker B, Lee, R, Newman K (2020) Optimizing nonsurgical treatments of overactive bladder in the United States. Urology 145: 52–9
Bulchandani S, Tooz-Hobson P, Verghese T, et al (2014) Does vaginal oestrogen treatment with support pessaries in vaginal prolapse reduce complications? Post Reprod Health 21(4): 141–5
Chung S, Kim W (2018) Various approaches and treatments for pelvic organ prolapse in women. J Menopausal Med 24: 155–62
Dhaliwal P, Wagg A (2016) Overactive bladder: strategies to ensure treatment compliance and adherence. Clin Interv Aging 11: 755–60
DeMaagd G, Davenport T (2012) Management of urinary incontinence. PT 37(6): 345-621
Dicker D, Alfadda A, Coutinho W, et al (2021) Patient motivation to lose weight: importance of healthcare professional support, goals and self-efficacy. Eur J Internal Med 91: 10–16
Domoney C (2014) Treatment of vaginal atrophy. Women’s Health 10(2): 191–200
Dwyer L, Stewart E, Rajai A (2021) A service evaluation to determine where and who delivers pessary care in the UK. Int J Urogynaecol 32(4): 1001–6
Faiena I, Patel N, Parihar JS, et al (2015) Conservative management of urinary incontinence in women. Rev Urol 17(3): 129–39
Fontaine C, Papworth E, Pascoe J (2021) Update on the management of overactive bladder. Ther Adv Urol 13: 17562872211
International Continence Society (2018) Stress Urinary Incontinence. Available online: www.ics.org/committees/standardisation/terminologydiscussions/sui
Jones K, Harmanli O (2010) Pessary use in pelvic organ prolapse and urinary incontinence. Rev Obstet Gynecol 3(1): 3–9
Mazur-Bialy A, Kolomanska-Bogucka D, Nowakowski C, Tim S (2020) Urinary incontinence in women: modern methods of physiotherapy as a support for surgical treatment or independent therapy. J Clin Med 9(4): 1211
NHS (2022) The NHS Digital Weight Management Programme. Available online: www.england.nhs.uk/digital-weightmanagement/
National Institute for Health and Care Excellence (2013) Urinary incontinence in women: management. CG171. NICE, London. Available online: www.nice.org.uk/guidance/cg171
National Institute for Health and Care Excellence (2017) Urinary Incontinence in Women: management clinical guideline. NICE, London. Available online: www.nice.org.uk/guidance/cg171
National Institute for Health and Care Excellence (2019a) Incontinence: urinary, in women; Antimuscarinics. NICE, London. Available online: https://cks.nice.org.uk/topics/incontinence-urinary-in-women/prescribing-information/antimuscarinics/
National Institute for Health and Care Excellence (2019b) Urinary incontinence and pelvic organ prolapse in women: management. NICE guideline [NG123]. NICE, London. Available online: www.nice.org.uk/guidance/ng123
National Institure for Health and Care Excellence (2021) Pelvic floor dysfunction: prevention and non-surgical management. NICE guideline [NG210]. NICE, London. Available online: www.nice.org.uk/guidance/ng210
National Institute for Health and Care Excellence/BNF (2022) Antimuscarinics (systemic). Available online: https://bnf.nice.org.uk/drug-class/antimuscarinicssystemic.html
National Institute for Health and Care Excellence/BNF (2022) Duloxetine. Available online: https://bnf.nice.org.uk/drug/duloxetine.html
Noble N (2018) Female urinary incontinence: pharmacological treatments. Nurse Prescribing 16(3): 116–20
Okeahialam N, Dworzynski K, Jacklin P, et al (2022) Prevention and non-surgical management of pelvic floor dysfunction: summary of NICE Guidelines. BMJ 376: n3049
Ostle Z (2016) Assessment, diagnosis and treatment of urinary incontinence in women. Br J Nurs 25(2): 84–91
Pomian A, Lisik W, Kosieradzki M (2016) Obesity and pelvic floor disorders: a review of the literature. Med Sci Monit 22: 1880–6
Rantell A (2015) Understanding urinary incontinence in women. Practice Nursing 26(6): 275–81
Sudol N, Adams-Piper E, Perry R, Lane F, Chen K (2019) In search of mobile applications for patients with pelvic floor disorders. Female Pelvic Med Reconstr 25(3): 252–6
Stewart E (2019) Urogynaecology. In: Holloway D, ed. Nursing management of women’s health: A guide for nurse specialists and practitioners. Springer: 215–34
United Kingdom Continence Society. UK Clinical Guideline: for best practice in the use of vaginal pessaries for pelvic organ prolapse (launched March 20221). Available online: www.ukcs.uk.net/UK-PessaryGuideline-2021
Vanichtantikul A, Tharavichitkul E, Chitapanarux I, Chinthakanan O (2017) Treatment of endometrial cancer in association with pelvic organ prolapse. Case Rep Obstet Gynecol 2017: 1640614
Zeiger B, Da Silva Carramao S, Del Roy C, et al (2021) Vaginal pessary in advanced pelvic organ prolapse: impact on quality of life. Int Urogynaecol J Nov 6: 1–8
This piece was first published in the Journal of General Practice Nursing. To cite this article use: Stewart E (2022) Treatments for female urinary incontinence and pelvic organ prolapse. J Gen Pract Nurs 8(1): 47-53