References
Abrams P, Cardozo L, Khoury S, Wein A (2012) 5th International Consultation on Incontinence, Paris, February 2012; 364
Anger JT, Saigal CS, Stothers L, et al (2006) The prevalence of urinary incontinence among community dwelling men: results from the National Health and Nutrition Examination survey. J Urol 176: 2103–8
Brodie A (2006) A guide to the management of one-piece urinary sheaths. Nurs Times 102(9): 49, 51
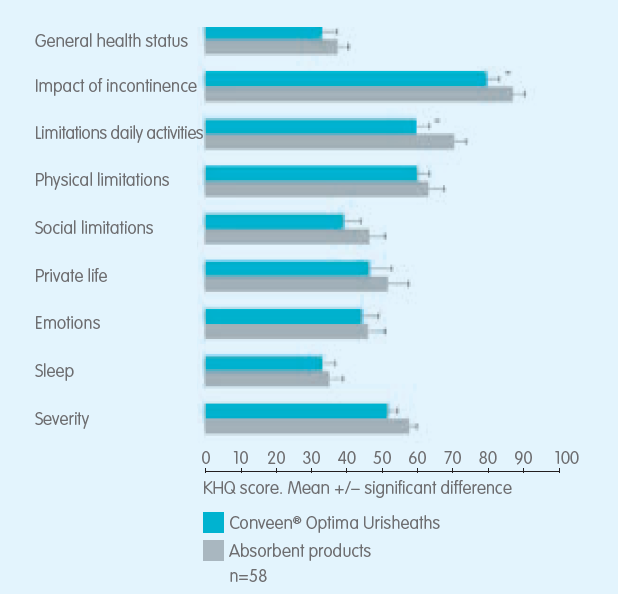
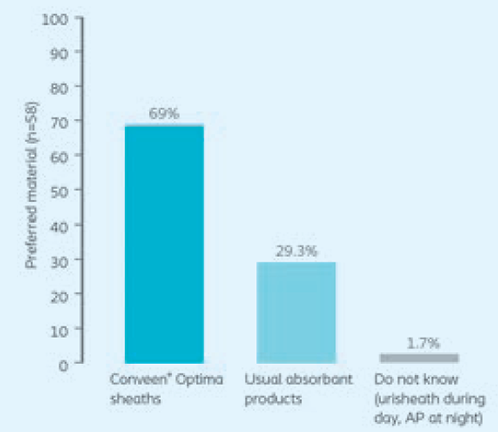
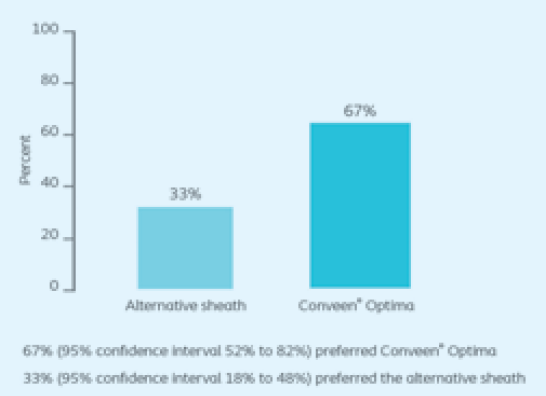
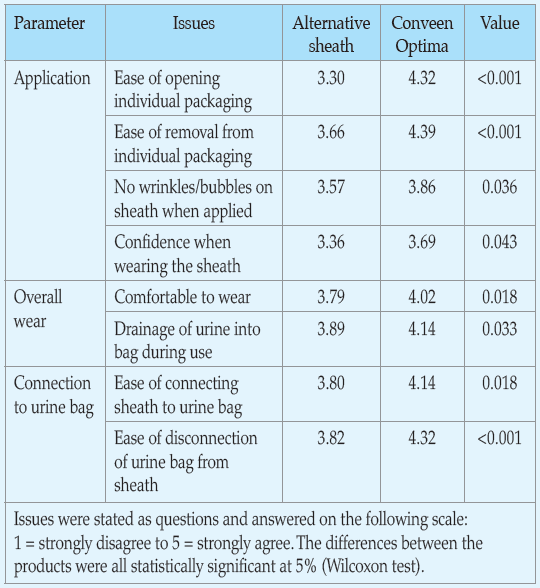
Chartier-Kastler E, Ballanger P, Petit J, et al (2011) Randomized, crossover study evaluating patient preference and the impact on quality of life of urisheaths vs absorbent products in incontinent men. BJU 108(2): 241–7
Gray M (2007) Incontinence-related skin damage: essential knowledge. Ostomy Wound Management 53(12): 28–32
Pemberton P, Brooks A, Eriksen CM, et al (2006) A comparative study of two types of urinary sheath. Nurs Times 102(7): 36–41
Shamliyan TA, Wyman JF, Ping R, Wilt TJ, Kane RL (2009) Male urinary incontinence: prevalence, risk factors, and preventive interventions. Rev Urol 11: 145–65
Williams D, Moran S (2006) Use of urinary sheaths in male incontinence. Nurs Times 102(47): 42
This piece was first published in the Journal of General Practice Nursing. To cite this article use: Supporting men with bladder incontinence (2022) J Gen Pract Nurs 8(3): 26-28