References
Behling M, Winters B (2021) Methods to stop caffeine use and minimize caffeine withdrawal symptoms in the state of caffeine dependence: a literature review. Available online: https://scholarsarchive.byu.edu/cgi/viewcontent.cgi?article=1363&context=studentpub
Evatt DP, Juliano L, Griffiths R (2016) A brief manualized treatment for problematic caffeine use: a randomized control trial. J Consult Clin Psychol 84(2): 113-121
Jura YH, Townsend MK, Curhan GC, Resnick NM, Grodstein F (2011) Caffeine intake, and the risk of stress, urgency and mixed urinary incontinence. J Urology 185(5): 1775-80
Le Berre M, Presse N, Morin M, et al (2020) What do we really know about the role of caffeine on urinary tract symptoms? A scoping review on caffeine consumption and lower urinary tract symptoms in adults, Neurourol Urodyn 39(5): 1217-1233
NHS inform (2021) Looking after your bones. Available online: https://www.nhsinform.scot/healthy-living/preventing-falls/keeping-well/looking-after-your-bones
Ogeil RP, Phillips JG (2015) Commonly used stimulants: sleep problems, dependence and psychological distress. Drug Alcohol Depend 153: 145-151
Roggeman S, Weiss JP, Van Laecke E, et al (2020) The role of lower urinary tract symptoms in fall risk assessment tools in hospitals: a review. F1000Research, 9: 1-8
Evatt DP, Juliano L, Griffiths R (2016) A brief manualized treatment for problematic caffeine use: a randomized control trial. J Consult Clin Psychol 84(2): 113-121
Jura YH, Townsend MK, Curhan GC, Resnick NM, Grodstein F (2011) Caffeine intake, and the risk of stress, urgency and mixed urinary incontinence. J Urology 185(5): 1775-80
Le Berre M, Presse N, Morin M, et al (2020) What do we really know about the role of caffeine on urinary tract symptoms? A scoping review on caffeine consumption and lower urinary tract symptoms in adults, Neurourol Urodyn 39(5): 1217-1233
NHS inform (2021) Looking after your bones. Available online: https://www.nhsinform.scot/healthy-living/preventing-falls/keeping-well/looking-after-your-bones
Ogeil RP, Phillips JG (2015) Commonly used stimulants: sleep problems, dependence and psychological distress. Drug Alcohol Depend 153: 145-151
Roggeman S, Weiss JP, Van Laecke E, et al (2020) The role of lower urinary tract symptoms in fall risk assessment tools in hospitals: a review. F1000Research, 9: 1-8



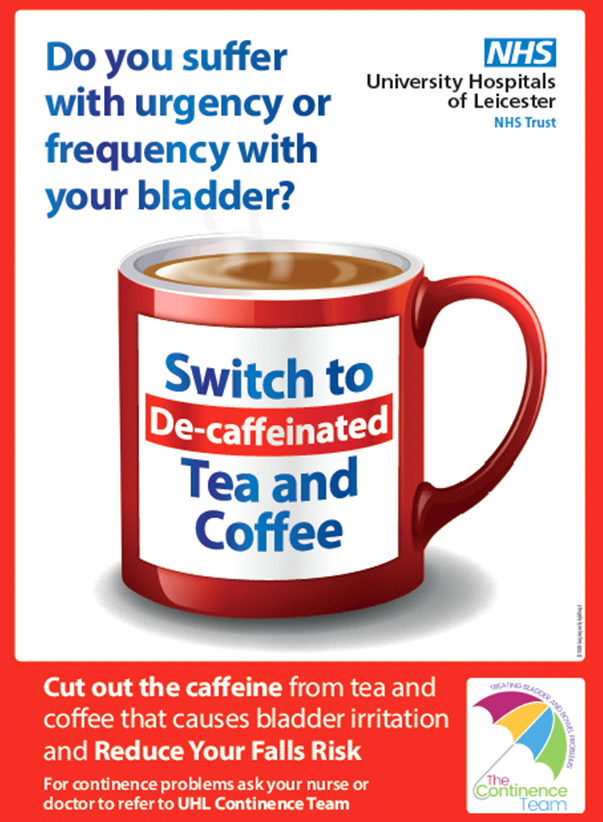
RushingToTheToiletPoster-Final.jpg)