References
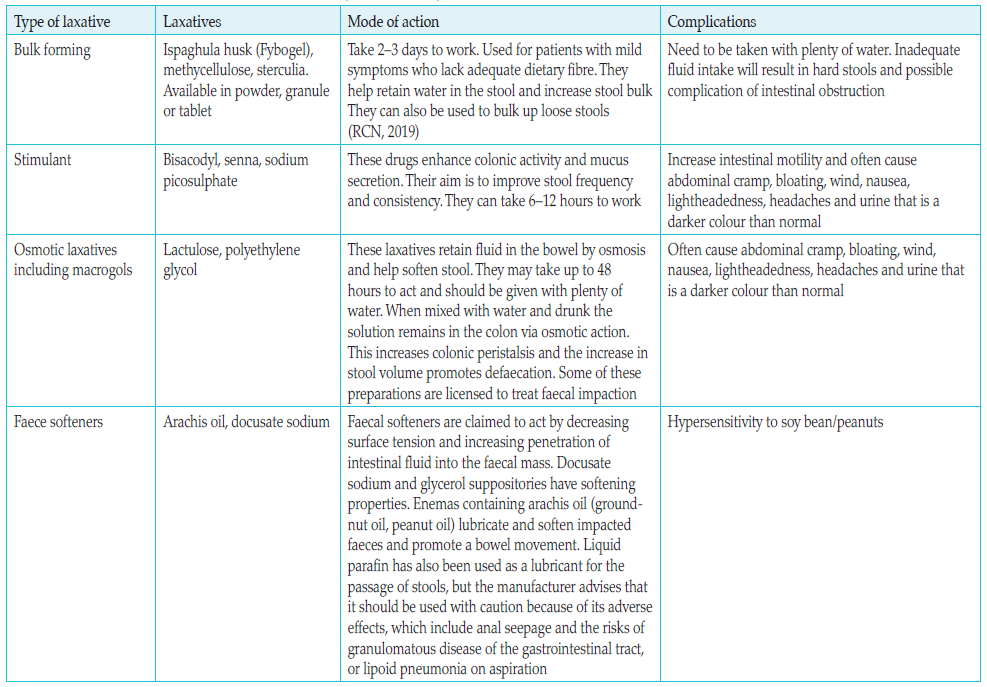
British National Formulary, National Institute for Health and Care Excellence (2021) Constipation | Treatment summary. BNF content published by NICE. Available online: https://bnf.nice.org.uk/treatment-summary/constipation.html
Booth J (2013) Continence care is every nurse’s business. Nurs Times 109(17– 18): 12–16
Burkhard FC, Bosch JLHR, Lemack AK, Nambiar N, et al (2020) European Association of Urology (EAU) Guidelines on Urinary Incontinence in Adults. Available online: https://uroweb.org/wp-content/uploads/EAU-Guidelines-Urinary-Incontinence-2016.pdf
Dementia UK (2017) Continence. Available online: www.dementiauk.org
Dumoulin C, Adewuyi T, Booth J, et al (2017) Adult conservative management. In: Abrams P, Cardozo L, Wagg A, Wein A, eds. Incontinence. 6th edn. Chap 12. Available online: https://www.ics.org/education/icspublications/icibooks
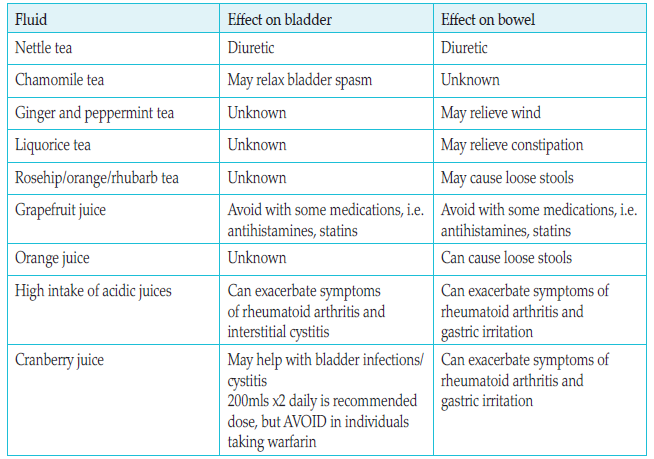
Gilbert R (2006) Fluid intake and bladder and bowel function. Nurs Times 102(12): 55
Goodman CI, Davies S, Norton C, et al (2013) Can district nurses and care home staff improve bowel care for older people using a clinical benchmarking tool? Br J Community Nurs 18(12): 580–7
Herbert J (2019) The conservative assessment and treatment of mixed urinary and anal incontinence in women: a multidisciplinary approach. Urol News 23(6)
International Continence Society (2015) Fact Sheets. A Background to Urinary and Faecal Incontinence. Available online: https://www.ics.org/folder/news-and-publications/ics-factsheets/d/ics-fact-sheets-2015
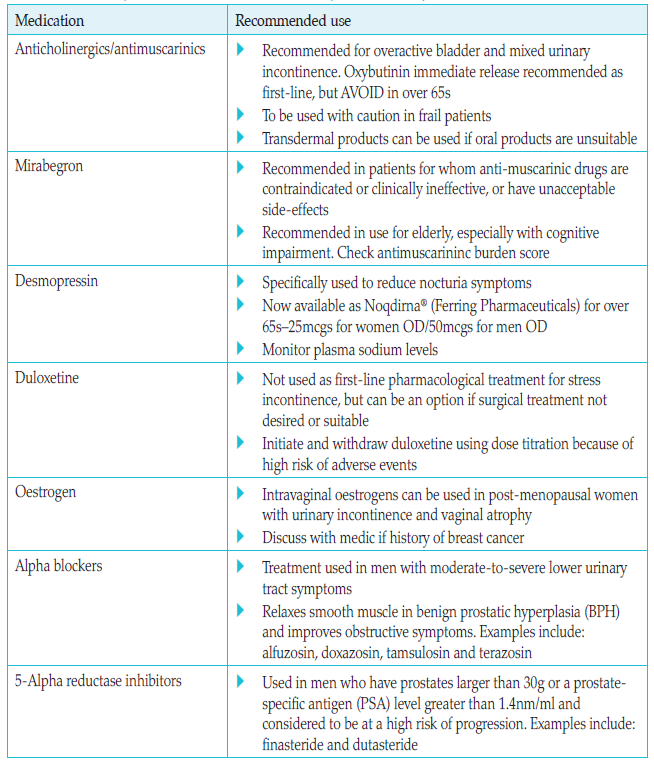
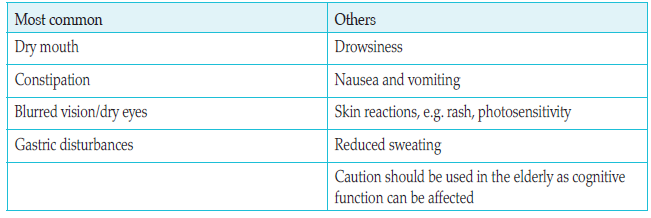
Madhuvrata P, Cody JD, Ellis G, Herbison GP, Hay-Smith EJC (2012) Which anticholinergic drug for overactive bladder symptoms in adults. Cochrane Database of Systematic Reviews 2012, Issue 1. Art. No.: CD005429. DOI: 10.1002/14651858. CD005429.pub2. Available online: www.cochrane.org/CD005429/INCONT_which-anticholinergic-drug-for-overactive-bladder-symptoms-in-adults
NHS Choices (2018) Bowel Incontinence. Available online: https://www.nhs.uk/live-well/eat-well/good-foods-to-help-your-digestion/
NHS (2019) Laxative overview. Available online: www.nhs.uk/conditions/laxatives/
National Institute for Health and Care Excellence (2013) Ulcerative colitis: management. CG 166. NICE, London. Available online: www.nice.org.uk/guidance/cg166
National Institute for Health and Care Excellence (2019) Urinary incontinence and pelvic organ prolapsed in Women: management. Clinical guideline 123. NICE, London. Available online: www.nice.org.uk/guidance/ng123
Royal College of Nursing (2019) Bowel Care. Management of Lower Bowel Dysfunction, including Digital Rectal Examination and Digital Removal of Faeces. Available online: www.rcn.org.uk/professional-development/publications/pub-007522
Toozs-Hobson P, Robinson D (2019) Managing the symptoms of overactive bladder. The Pharmaceutical Journal, 8 March. Available online: https://pharmaceutical-journal.com/article/ld/managing-the-symptoms-of-overactive-bladder
Yates A (2016) The importance of good continence care for older people. Nurs Res Care 18(10): 532–6
Yates A (2019) Female pelvic floor 2: assessment and rehabilitation. Nurs Times (online) 115(6): 30–3