Resources
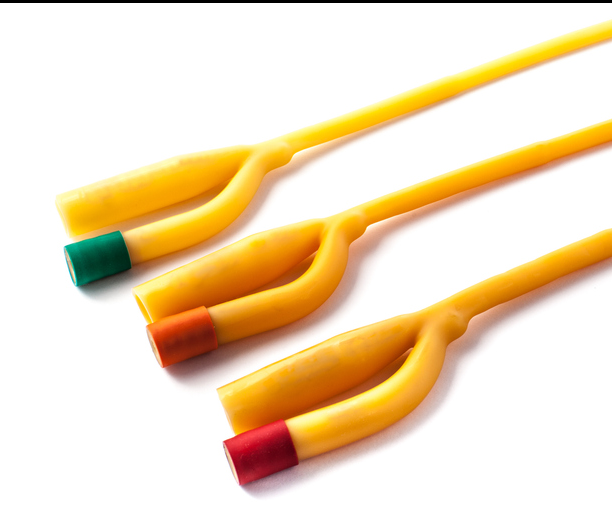
The fourth and final part of the continence clinical skills series identifies how continence problems, which may not have responded to conservative treatment/ interventions, can be managed by the appropriate use of equipment/devices and products. The range available is vast and variable and some are more suitable to specific conditions than others. Healthcare professionals need to understand how they work to offer the best solution for individuals and their lifestyle. Products include, for example, commodes, urinals, sheaths, catheters, anal irrigation and pad products. This article specifically looks at equipment/devices and products for urinary retention, e.g. catheters; urinary incontinence, e.g. sheaths, pubic pressure devices; and faecal incontinence, e.g. anal plugs, transanal irrigation (TAI) and pad products.

.png)