Resources
Helen Lake is Urology Specialist Nurse and UTI Information Nurse, The Urology Foundation
Dr Nicola Adanna Okeahialam, Professor Fiona Reid
Women presenting with stress urinary incontinence or pelvic organ prolapse face an increasingly complex landscape of treatment options. Owing to a lack of clear superiority between treatment options for pelvic organ prolapse and stress urinary incontinence, the decision about which surgical procedure will be performed is a ‘preference sensitive’ decision, requiring careful consideration of each patient’s values and goals. However, the process of making a decision about treatment can be challenging because of a number of factors including patient understanding, clinician preferences and institutional barriers. In line with principles outlined in Montgomery v Lanarkshire Health Board [2015] and following the recommendations of the Cumberlege report, a collaborative approach to shared decision making is essential, to identify both what matters most to patients and also the material risks. This can be achieved by using patient decision aids to supplement consultations and support patients to reach an informed and preference-sensitive decision regarding surgery.
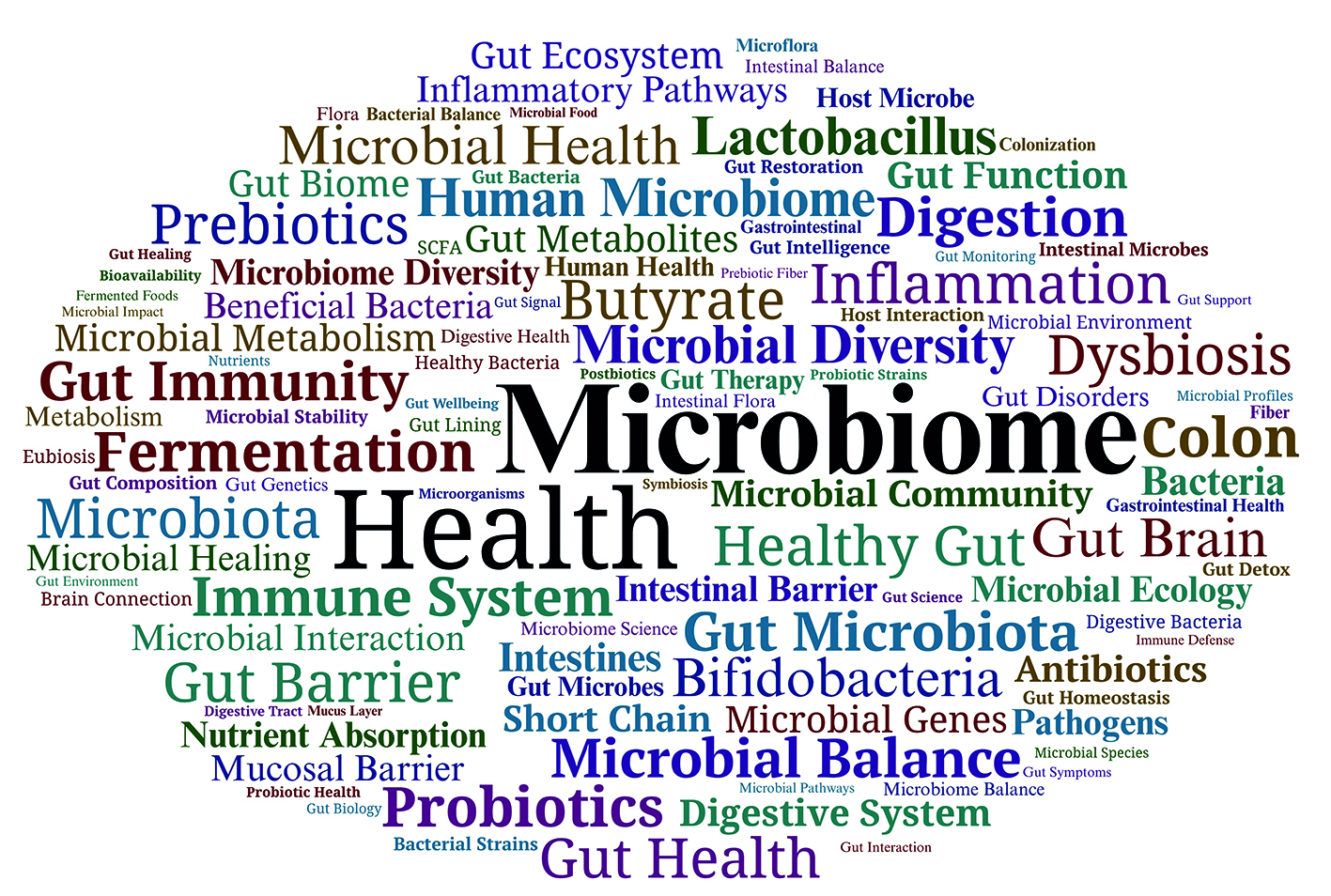
Key words: Gut microbiome; Physical and mental wellbeing; Healthy microbiota; Dysbiosis; Gut–brain axis