References
Almuhaideb M, Bandaru D, Chawareb EA, Yafi FA, Hammad MAM (2025) Ethical perspective on telemedicine usage in sexual medicine: A friend or a foe? UroPrecision. 3:47–53. https://doi.org/10.1002/uro2.111
Healthcare Business Solutions (UK) Ltd (2025a) Digital Healthcare and Insourcing’s Role in Achieving the NHS Net Zero Target: HBSUK Perspectives. https://www.hbsuk.co.uk/sustainability-whitepaper/ (accessed 23 December 2025)
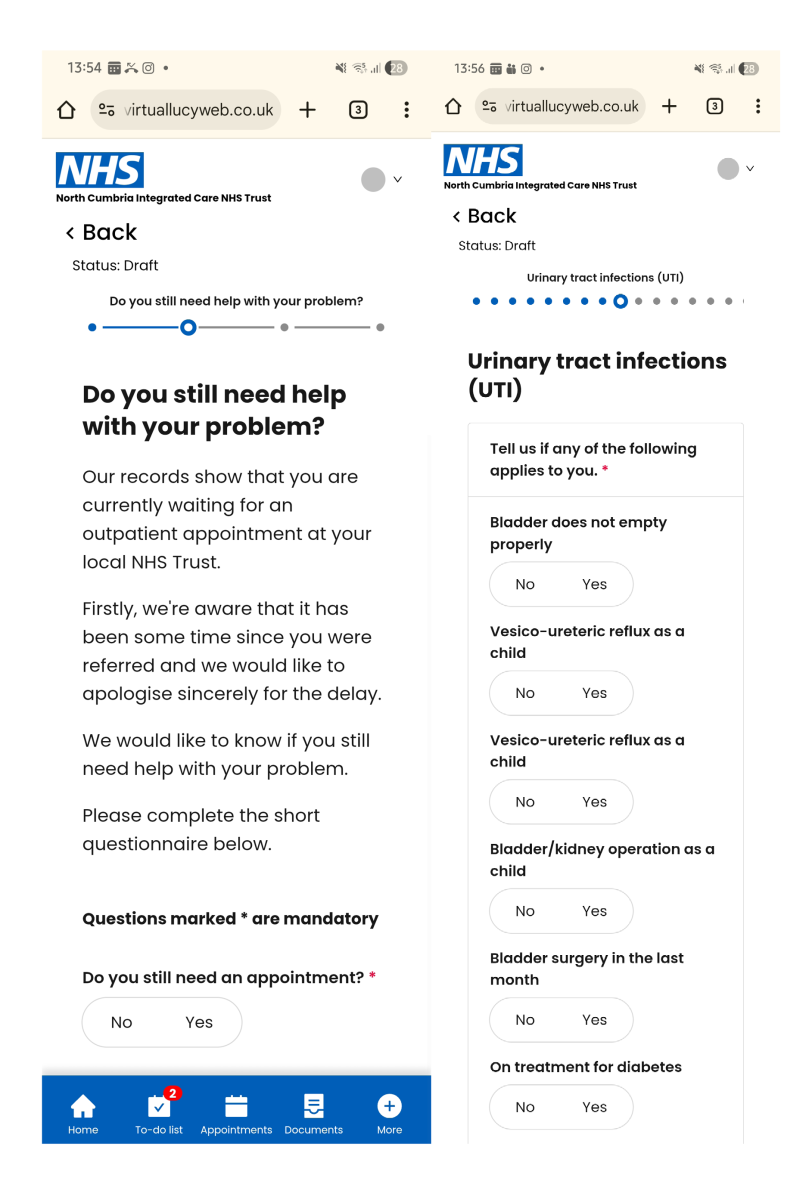
Healthcare Business Solutions (UK) Ltd (2025b) How online assessments drove a 35% reduction in urology waiting lists. https://www.hbsuk.co.uk/case-studies/ncic-urology/ (accessed 12 December 2025)
Lundon D (2023) Telehealth in Urology. https://doi.org/10.1016/C2020-0-04179-4 (accessed 12 December 2025)
Moulaei K, Kazemi-Arpanahi H (2025) Applications, benefits, and challenges of adopting teleurology: a scoping review. World J Urol. 43(1):330. https://doi.org/10.1007/s00345-025-05706-1
Moulaei K, Sheikhtaheri A, Fatehi F, Shanbehzadeh M, Bahaadinbeigy K (2023) Patients' perspectives and preferences toward telemedicine versus in-person visits: a mixed-methods study on 1226 patients. BMC Med Inform Decis Mak. 23(1):261. https://doi.org/10.1186/s12911-023-02348-4
Naik N, Nandyal SR, Nayak SG et al (2022) Telemedicine and telehealth in urology: uptake, impact and barriers to clinical adoption. Front Surg. 9:911206. https://doi.org/10.3389/fsurg.2022.911206
Okoye F, Gadzinski AJ, Sekar R et al (2024) Telemedicine for multidisciplinary urologic cancer care: a prospective single institution study. Clin Genitourin Cancer. 22(3):102058. https://doi.org/10.1016/j.clgc.2024.02.009
Seckam A (2023) Does digital health revolutionise medical practice? J Commun Nurs. 37(4):22-23
Seckam A, Mitchell S (2025) Technological developments in urology. https://www.ucc-today.com/journals/issue/launch-edition/article/technological-developments-in-urology (accessed 12 December 2025)
Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, Caffery LJ (2020) Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 26(5):309-313. https://doi.org/10.1177/1357633X20916567
Healthcare Business Solutions (UK) Ltd (2025a) Digital Healthcare and Insourcing’s Role in Achieving the NHS Net Zero Target: HBSUK Perspectives. https://www.hbsuk.co.uk/sustainability-whitepaper/ (accessed 23 December 2025)
Healthcare Business Solutions (UK) Ltd (2025b) How online assessments drove a 35% reduction in urology waiting lists. https://www.hbsuk.co.uk/case-studies/ncic-urology/ (accessed 12 December 2025)
Lundon D (2023) Telehealth in Urology. https://doi.org/10.1016/C2020-0-04179-4 (accessed 12 December 2025)
Moulaei K, Kazemi-Arpanahi H (2025) Applications, benefits, and challenges of adopting teleurology: a scoping review. World J Urol. 43(1):330. https://doi.org/10.1007/s00345-025-05706-1
Moulaei K, Sheikhtaheri A, Fatehi F, Shanbehzadeh M, Bahaadinbeigy K (2023) Patients' perspectives and preferences toward telemedicine versus in-person visits: a mixed-methods study on 1226 patients. BMC Med Inform Decis Mak. 23(1):261. https://doi.org/10.1186/s12911-023-02348-4
Naik N, Nandyal SR, Nayak SG et al (2022) Telemedicine and telehealth in urology: uptake, impact and barriers to clinical adoption. Front Surg. 9:911206. https://doi.org/10.3389/fsurg.2022.911206
Okoye F, Gadzinski AJ, Sekar R et al (2024) Telemedicine for multidisciplinary urologic cancer care: a prospective single institution study. Clin Genitourin Cancer. 22(3):102058. https://doi.org/10.1016/j.clgc.2024.02.009
Seckam A (2023) Does digital health revolutionise medical practice? J Commun Nurs. 37(4):22-23
Seckam A, Mitchell S (2025) Technological developments in urology. https://www.ucc-today.com/journals/issue/launch-edition/article/technological-developments-in-urology (accessed 12 December 2025)
Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, Caffery LJ (2020) Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 26(5):309-313. https://doi.org/10.1177/1357633X20916567